Professional Documents
Culture Documents
Neurocardiogenic Syncope PDF
Uploaded by
Anonymous HrEatuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neurocardiogenic Syncope PDF
Uploaded by
Anonymous HrEatuCopyright:
Available Formats
Arrhythmias
Neurocardiogenic Syncope: When and Focused Review
How to Treat?
afforded considerable latitude in planning therapy based on
Blair Grubb, MD and Daniel J. Kosinski, MD, the patient’s clinical circumstance.
Electrophysiology Section, Division of Cardiology, In addition, it is our opinion that any patient with
Department of Medicine, The Medical College of Ohio, neurocardiogenic syncope and clinical episodes that occur
Toledo, Ohio while in the seated position require treatment. These pa-
tients are at risk for syncope during activities such as
Neurocardiogenic syncope is a very common cause of syn- driving or operating other vehicles, industrial equipment,
etc. In these individuals, the customary method of lying
cope. In some patient populations, such as children and
down in order to abort an episode is often ineffective and/or
adolescents, it is the most common cause of syncope. Yet,
unrealistic.
despite numerous publications on the subject, decisions on
treatment of the disorder remain ambiguous.
In patients with frequent episodes of neurocardiogenic Treatment
syncope, the decision to treat is obvious. However, in Numerous treatment modalities have been shown to be
patients with a single or infrequent episode(s), the decision effective in neurocardiogenic syncope. The physician must
to treat is often times very difficult. If such patients have a choose a treatment plan based on the patient’s age, tilt
clear precipitant, such as phlebotomy, treatment beyond response, comorbidities and other medications the patient
education may not be necessary. In most patients with a may be taking.
single or infrequent episode(s), we look principally at two If at all possible, nonpharmacologic treatment should be
clinical factors. The first factor we consider is whether or employed. The first issue to consider is whether or not the
not a reasonable prodrome of symptoms occurred prior to patient is taking medication that can be prosyncopal. Such
syncope. The second clinical factor is the lifestyle and/or medications would include diuretics, vasodilators and/or
occupation of the patient. For instance, a patient with a centrally acting agents such as MAO inhibitors or tricyclic
sedentary lifestyle and two syncopal episodes usually does antidepressants. If such medications can safely be reduced
not require treatment if the episodes occur with a 30 – 60 or withdrawn, this should be considered.
second prodrome. This would allow the patient time to sit Education should be provided encouraging the patient
or lie down and thus avoid injury. Conversely, a truck to avoid volume depletion. The patient should be advised to
driver with a single episode would be appropriate to treat if moderately increase salt intake and to sit or lie down at the
the episode occurred with little or no prodrome. We realize first sign of an impending event. However, this type of
these guidelines are vague. However, the decision to treat in advice is sometimes unhelpful. Some patients have little or
these cases is often difficult, and physicians should be no prodrome warning and in other patients, salt loading
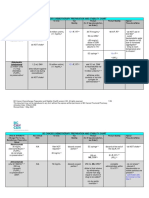
Table 1. Therapy for neurocardiogenic syncope
Medication/Typical Dose Mechanism of Action Advantages Disadvantages
Fludrocortisone .1–.4 mg/qd Volume expansion; Relatively safe; reasonably priced Headache; potential for hypokalemia
vasoconstriction
-blocker therapy Contraindicated in some patients;
-Inderal 80–160 mg qd -adrenergic blockage relatively safe; reasonable cost inappropriate for patients with
-metoprolol 50–100 mg qd severe bradycardic episodes
Midodrine 5–10 mg tid Alpha agonist; Very effective Supine hypertension; tid dosing;
vasoconstriction headache
Methylphenidate 5–10 mg tid Vasoconstriction May benefit patients with fatigue; Headache; stimulant side effects;
stimulant properties addictive potential
Clonidine .1–.3 mg bid Centrally acting agent Safe in hypertensive patients Orthostatic hypotension
SSRI drugs
Zoloft 50 mg qd Serotonin reuptake inhibition Once daily dosing; generally safe Plethora of side effects
Prozac 20 mg qd
Paxil 20 mg qd
Yohimbine 8 mg bid–tid Uncertain May be useful in refractory Anxiety; nervousness
cases—not a firstline therapy
Erythropoietin 4,000 IU sq bi-weekly Uncertain May be useful in refractory Requires injections; inconvenient;
cases—not a firstline agent expensive
Disopyramide 100–200 mg bid of Negative inotropic; Can be effective in refractory Requires drug level monitoring; side
sustained release anticholinergic properties cases—not a first line agent effects can be serious
ACC CURRENT JOURNAL REVIEW Mar/Apr 2001
© 2001 by the American College of Cardiology 1062-1458/01/$20.00
Published by Elsevier Science Inc. 67 PII S1062-1458(01)00215-X
and/or volume expansion may be inadvisable for other Summary
reasons such as supine hypertension.
Nonpharmacologic therapy can include elastic support In patients with neurocardiogenic syncope, decisions on
hose. These hose should best be ordered to be thigh high when to treat and how to treat are based more on individual
with 30 – 40 mm Hg counter pressure. However, this form issues than randomized trial data. Although guidelines do
of therapy has several drawbacks including aesthetic issues exist, a premium remains on thoughtful clinical judgment
and issues of comfort. tailored to the patient’s circumstance.
Finally, in some patients, orthostatic training, provided
by standing upright against a wall twice daily for varying Suggested Reading
amounts of time, may be useful. Kosinski D, Grubb BP. Vasodepressor syncope. Current Treat-
ment Options in Cardiovascular Medicine 2000; 2:309 –15.
Pharmacologic Therapy Bloomfield D, Sheldon R, Grubb BP, et al. Putting it all together: A
new treatment algorithm for vasovagal syncope and related
A summary of various pharmacologic options is listed in disorders. Am J Cardiol 1999;84:33Q–9Q.
Table 1. While choosing a particular therapy, attention Connolly S, Sheldon R, Roberts M. The North American vasovagal
must be paid to several factors. The physician must con- pacemaker study. A randomized trial of permanent cardiac
sider the patient’s age, other illnesses and medications, side pacing for the prevention of vasovagal syncope. J Am Coll
effects and compliance issues. Cardiol 1999;33:16 –20.
Cox M, Peelman B, Mayor R. Acute and long-term -adrenergic
blockade for patients with neurocardiogenic syncope. J Am
Cardiac Pacing Coll Cardiol 1995;26:1293– 8.
The role of cardiac pacing to treat neurocardiogenic syn- Grubb BP, Kosinski D, Boehm K, Kip K. Postural orthostatic
tachycardia syndrome: A neurocardiogenic variant identified
cope remains controversial. It is reserved for patients in
during head up tilt testing. PACE 1997;20:2205–12.
whom episodes include a substantial bradycardic compo- DiGirolamo E, DiForio C, Leonizio L, et al. Usefulness of a tilt
nent. In general, these patients are also refractory to phar- training program for the prevention of refractory neurocardio-
macologic therapy. However, some patients may prefer genic syncope in adolescents. Circulation 1999;100:1798 –
pacing to medical therapy. 801.
When pacing is utilized, a dual-chamber pacer with Grubb BP, Kosinski D. Dysautonomic and reflex syncope syn-
hysteresis or rate-drop function should be utilized. In ad- dromes. Cardio Clinics 1997;15:257– 63.
dition, patients should be advised that pacing alone may be
Address correspondence and reprint requests to Daniel J. Kosinski,
ineffective and that they may require adjunctive medical MD, Cardiology, Room 1192, The Medical College of Ohio, 3000 Arling-
treatment. ton Avenue, Toledo, OH 43614.
ACC CURRENT JOURNAL REVIEW Mar/Apr 2001
68
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Pharmacy Management SynopsisDocument7 pagesPharmacy Management SynopsisHariom75% (4)
- Doxorubicin/Cisplatin Protocol for OsteosarcomaDocument6 pagesDoxorubicin/Cisplatin Protocol for OsteosarcomaDenny LukasNo ratings yet
- Epic Armageddon: Adeptus MechanicusDocument19 pagesEpic Armageddon: Adeptus MechanicusSam Nice100% (1)
- Rasakarpoorantimicrobialrs PDFDocument228 pagesRasakarpoorantimicrobialrs PDFravi100% (1)
- Sfda GuideDocument1,540 pagesSfda Guidecelecosib100% (1)
- Ghallamore Incursion 3.0Document4 pagesGhallamore Incursion 3.0Anonymous HrEatuNo ratings yet
- Zone Mortalis PDFDocument13 pagesZone Mortalis PDFcarneraNo ratings yet
- Adeptus MechAdeptus Mechanicus Heavy Cruisersanicus Heavy CruisersDocument1 pageAdeptus MechAdeptus Mechanicus Heavy Cruisersanicus Heavy CruisersAnonymous HrEatuNo ratings yet
- Adeptus Mechanicus BattleshipsDocument1 pageAdeptus Mechanicus BattleshipsAnonymous HrEatuNo ratings yet
- Neurocardiogenic Syncope PDFDocument2 pagesNeurocardiogenic Syncope PDFAnonymous HrEatuNo ratings yet
- Ghallamore Incursion 3.0Document4 pagesGhallamore Incursion 3.0Anonymous HrEatuNo ratings yet
- Gargant Big Mob Reference SheetDocument2 pagesGargant Big Mob Reference SheetAnonymous HrEatuNo ratings yet
- BFG FAQ ExtensionDocument170 pagesBFG FAQ ExtensionAnonymous HrEatuNo ratings yet
- BFG FAQ ExtensionDocument170 pagesBFG FAQ ExtensionAnonymous HrEatuNo ratings yet
- Skills Matrix: Name / SkillDocument4 pagesSkills Matrix: Name / SkillAnonymous HrEatuNo ratings yet
- HierophantDocument4 pagesHierophantrhasputineNo ratings yet
- Pharma White PaperDocument13 pagesPharma White PaperAnonymous HrEatuNo ratings yet
- HierophantDocument4 pagesHierophantrhasputineNo ratings yet
- Vincristine (OncovinDocument4 pagesVincristine (Oncovin9959101161No ratings yet
- Synopsis FinalDocument11 pagesSynopsis FinalIshwari DeshmukhNo ratings yet
- Natco PipelineDocument5 pagesNatco Pipelinenikesh.nikzagNo ratings yet
- Translated From Original Russian Instructions by Extrapharmacy Online StoreDocument1 pageTranslated From Original Russian Instructions by Extrapharmacy Online StoreFaiz AmriNo ratings yet
- NO Kodebarang Satuan Pakai Stock Awal Masuk Keluar Stock Akhir Harga KeteranganDocument4 pagesNO Kodebarang Satuan Pakai Stock Awal Masuk Keluar Stock Akhir Harga Keteranganruang belajar farmasiNo ratings yet
- Sterilizers of ParenteralsDocument42 pagesSterilizers of ParenteralsHanuma KanthetiNo ratings yet
- Senior Director Bioprocess Development in Northern California Resume Venkatesh SrinivasanDocument4 pagesSenior Director Bioprocess Development in Northern California Resume Venkatesh SrinivasanVenkateshSrinivasan1No ratings yet
- Vendor Purchase With Date 2020Document8 pagesVendor Purchase With Date 2020Tunde AdeniranNo ratings yet
- LH 4 Physician Prescribing HabitsDocument14 pagesLH 4 Physician Prescribing HabitsDrRavi Mittal100% (1)
- Mdma by HPLCDocument5 pagesMdma by HPLCCarolmariaNo ratings yet
- Chemo Stability Chart - AtoKDocument59 pagesChemo Stability Chart - AtoKAfifah Nur Diana PutriNo ratings yet
- Report on Medicine StockDocument15 pagesReport on Medicine StockreyNo ratings yet
- 33 Cisplatin A ReviewDocument18 pages33 Cisplatin A Reviewtrifamonika23No ratings yet
- JURISPRUDENCE Unit-1 Bachlor of PharmacyDocument17 pagesJURISPRUDENCE Unit-1 Bachlor of PharmacySachin NagarNo ratings yet
- Tapasya Product CatalogueDocument104 pagesTapasya Product Cataloguethaonguyendc100% (1)
- 7779087Document65 pages7779087MohamedNo ratings yet
- Utami 2020 J. Phys. Conf. Ser. 1563 012024Document9 pagesUtami 2020 J. Phys. Conf. Ser. 1563 012024Whaler PausNo ratings yet
- Marketing Plan B6 BioconDocument9 pagesMarketing Plan B6 BioconRitvik DineshNo ratings yet
- Q-Absorbance Ratio Spectrophotometric Method For The Simultaneous Estimation of Rifampicin and Piperine in Their Combined Capsule DosageDocument5 pagesQ-Absorbance Ratio Spectrophotometric Method For The Simultaneous Estimation of Rifampicin and Piperine in Their Combined Capsule Dosagemahatir muhammadNo ratings yet
- TTTTDocument26 pagesTTTTMoataz TrabehNo ratings yet
- Novo's internationalization strategy through strategic JVs and acquisitionsDocument3 pagesNovo's internationalization strategy through strategic JVs and acquisitionsAbhishek NayakNo ratings yet
- 2013 Source BookDocument172 pages2013 Source BookAlex EspinozaNo ratings yet
- Form 19-CDocument15 pagesForm 19-Cs.sabapathyNo ratings yet
- 6-Gingerol ArecolineDocument8 pages6-Gingerol Arecolineapi-327826901No ratings yet
- CYMBALTA (Duloxetine HCL) Product Monograph For CanadaDocument49 pagesCYMBALTA (Duloxetine HCL) Product Monograph For Canadajennabush100% (10)
- 3 Analgesic Anitpyretic InfamDocument10 pages3 Analgesic Anitpyretic InfamAnonymous dRAu54No ratings yet