Professional Documents
Culture Documents
ACLS Chart
Uploaded by
Jev DespiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ACLS Chart
Uploaded by
Jev DespiCopyright:
Available Formats
MT 27-29 ACLS 07.17.
qxd 7/14/06 9:24 PM Page 3
Table 1. Medications Used for Adults in Pulseless Arrest
Drugs are de-emphasized in the new guidelines for resuscitation, but below are some facts you need to know.
Classification Out of Favor Recommendations Dosage Comments
Vasopressors High-dose Epinephrine for VF/pulseless 1 mg IV/IO every 3 to 5 minutes (higher doses The Committee considered removing
epinephrine VT may be used in the vasopressors from the pulseless arrest algorithm;
and asystole/PEA case of overdose from beta- or however, because of the
calcium-channel blockers.) possible benefits for short-term survival and the
lack of a placebo versus vasopressor trial, they
One dose of vasopressin 40 U IV or IO may be were kept in.
substituted for either the first or second dose of
epinephrine but has not been shown to improve
survival.
Antiarrhythmics Antiarrhythmics other Amiodarone for VF/pulseless Amiodarone 300 mg IV or IO, once, then con- Amiodarone is the only antiarrhythmic that has
than amiodarone, such VT sider additional 150 mg. been shown to improve
as procainamide, for (lidocaine remains accept- short-term outcome, but even it did not improve
VF and pulseless VT able to use.) A new aqueous formulation has reduced the survival to hospital discharge.
incidence of hypotension associated with this
drug.
Atropine for asystole/slow 1 mg IV or IO, repeat every 3 to 5 minutes up
PEA to three doses.
Magnesium for 1 to 2 g diluted in 10 mL D5W IV
torsades de pointes or IO push over 5 to 20 minutes
KEY
VF = ventricular fibrillation VT = ventricular tachycardia PEA = pulseless electrical activity IO = intraosseous
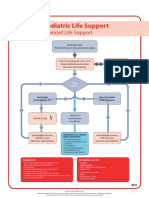
PULSELESS ARREST
• BLS Algorithm: Call for help, give CPR
• Give oxygen when available
• Attach monitor/defibrillator when available
2
Shockable Check rhythm Not Shockable
3 Shockable rhythm? 9
VF/VT Asystole/PEA
4
Give 1 shock
• Manual biphasic: device specific
(typically 120 to 200 J)
10
Note: If unknown, use 200 J
Resume CPR immediately for 5 cycles
• AED: device specific When IV/IO available, give vasopressor
• Monophasic: 360 J • Epinephrine 1 mg IV/IO
Resume CPR immediately Repeat every 3 to 5 min
or
• May give 1 dose of vasopressin 40 U IV/IO to
5 Give 5 cycles of CPR*
replace first or second dose of epinephrine
Check rhythm No Consider atropine 1 mg IV/IO
Shockable rhythm? for asystole or slow PEA rate
Repeat every 3 to 5 min (up to 3 doses)
6 Shockable
Continue CPR while defibrillator is charging
Give 1 shock Give 5 cycles
• Manual biphasic: device specific of CPR*
(same as first shock or higher dose)
Note: If unknown, use 200 J 11
• AED: device specific
• Monophasic: 360 J Check rhythm
Resume CPR immediately after the shock Shockable rhythm?
When IV/IO available, give vasopressor during CPR
(before or after the shock)
• Epinephrine 1 mg IV/IO
Repeat every 3 to 5 min
or
• May give 1 dose of vasopressin 40 U IV/IO to
12
replace first or second dose of epinephrine
Not
13
• If asystole, go to Box 10
• If electrical activity, check Shockable Shockable Go to
Give 5 cycles of CPR* pulse. If no pulse, go to
7 Box 4
Box 10
Check rhythm No • If pulse present, begin
Shockable rhythm? postresuscitation care
Shockable
8 During CPR
Continue CPR while defibrillator is charging • Push hard and fast (100/min) • Rotate compressors every
Give 1 shock • Ensure full chest recoil 2 minutes with rhythm checks
• Manual biphasic: device specific • Search for and treat possible
(same as first shock or higher dose) • Minimize interruptions in chest
compressions contributing factors:
Note: If unknown, use 200 J – Hypovolemia
• AED: device specific • One cycle of CPR: 30 compressions – Hypoxia
• Monophasic: 360 J then 2 breaths; 5 cycles ≈2 min – Hydrogen ion (acidosis)
Resume CPR immediately after the shock • Avoid hyperventilation – Hypo-/hyperkalemia
Consider antiarrhythmics; give during CPR – Hypoglycemia
• Secure airway and confirm placement – Hypothermia
(before or after the shock)
amiodarone (300 mg IV/IO once, then – Toxins
– Tamponade, cardiac
consider additional 150 mg IV/IO once) or
lidocaine (1 to 1.5 mg/kg first dose, then 0.5 to
* After an advanced airway is placed,
rescuers no longer deliver “cycles” – Tension pneumothorax
0.75 mg/kg IV/IO, maximum 3 doses or 3 mg/kg) of CPR. Give continous chest com- – Thrombosis (coronary or
Consider magnesium, loading dose pressions without pauses for breaths. pulmonary)
Give 8 to 10 breaths/minute. Check – Trauma
1 to 2 g IV/IO for torsades de pointes
After 5 cycles of CPR,* got to Box 5 above rhythm every 2 minutes
© 2005 American Heart Association
July 17, 2006 MT | www.nurseweek.com 29
You might also like
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- Pediatric Cardiac Arrest and Bradycardia AlgorithmsDocument6 pagesPediatric Cardiac Arrest and Bradycardia AlgorithmsandiyanimalikNo ratings yet
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDocument49 pagesAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamNo ratings yet
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- (Advanced Cardiac Life Support) : ACLS Algorithms 2018Document18 pages(Advanced Cardiac Life Support) : ACLS Algorithms 2018cristina100% (1)
- Rhythm Recognition - ACLS Medical Training 1Document9 pagesRhythm Recognition - ACLS Medical Training 1Catalina BorquezNo ratings yet
- CPR AED Choking Guidelines for Healthcare ProvidersDocument2 pagesCPR AED Choking Guidelines for Healthcare Providersreyes markNo ratings yet
- Megacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...Document1 pageMegacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...krgduraiNo ratings yet
- ACLS Written 2006 Precourse Self AssessmentDocument14 pagesACLS Written 2006 Precourse Self AssessmentmonickamsNo ratings yet
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyNo ratings yet
- ACLS and PALS Certification Practice QuestionsDocument11 pagesACLS and PALS Certification Practice Questionsdyah rahayu hutamiNo ratings yet
- ACLS Algorithms SlideDocument26 pagesACLS Algorithms SlidehrsoNo ratings yet
- ACLS Study GuideDocument28 pagesACLS Study GuideNicole Berry100% (1)
- ACLS ECG Strip Interpretation and Study GuideDocument12 pagesACLS ECG Strip Interpretation and Study GuideMariana Berger100% (1)
- Nursing Responsibilities in Handling AntibioticsDocument4 pagesNursing Responsibilities in Handling Antibioticsrichardmd20% (1)
- ACLS Training - Most Important Points To RememberDocument5 pagesACLS Training - Most Important Points To RememberEman ElzeftawyNo ratings yet
- ACLS Algorithm GuideDocument1 pageACLS Algorithm GuideAhmed AlkhaqaniNo ratings yet
- Normal Ranges Vital Signs 2017Document2 pagesNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- ICE DrugsDocument2 pagesICE DrugsRichelle FrondaNo ratings yet
- Introd To ECG Code Blue Champs March 2019Document52 pagesIntrod To ECG Code Blue Champs March 2019james rukenya100% (1)
- Basic Life Support (BLS) Training Course: FeaturesDocument1 pageBasic Life Support (BLS) Training Course: FeaturesSheryl Fuentes De GuzmanNo ratings yet
- 15 item ACLS Drill ReviewDocument4 pages15 item ACLS Drill ReviewVal SolidumNo ratings yet
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- Calc Drip Rates 2Document2 pagesCalc Drip Rates 2Charisse Nicole DiazNo ratings yet
- AHA ELearning ACLS Precourse Self-Assessment and Precourse WorkDocument1 pageAHA ELearning ACLS Precourse Self-Assessment and Precourse Work9kjsntkrzcNo ratings yet
- IU Health ACLS Study GuideDocument8 pagesIU Health ACLS Study Guideeng78ineNo ratings yet
- Dysrhythmia TestsDocument3 pagesDysrhythmia TestsKimberly WhitesideNo ratings yet
- Pharmacology For Paramedics: Jeremy Maddux, NREMTP, I/CDocument215 pagesPharmacology For Paramedics: Jeremy Maddux, NREMTP, I/CSreejesh RkNo ratings yet
- 2010 Integrated Updated Circulation ACLS Acute Coronary Syndromes AlgorithmDocument1 page2010 Integrated Updated Circulation ACLS Acute Coronary Syndromes Algorithmms_lezahNo ratings yet
- The Crash CartDocument39 pagesThe Crash Cartpramod kumawat100% (1)
- ACLS QuizletDocument7 pagesACLS Quizletek.9006001No ratings yet
- ECG Master Class-2Document138 pagesECG Master Class-2Shohag ID Center100% (1)
- Arrhythmia Recognition Poster Part 2Document1 pageArrhythmia Recognition Poster Part 2Gwen LylesNo ratings yet
- PALS Precourse Self 2023Document9 pagesPALS Precourse Self 2023Airene SibleNo ratings yet
- ACLS and MegacodeDocument33 pagesACLS and MegacodeMark Joseph100% (1)
- ACLS Simplify AlgorithmDocument6 pagesACLS Simplify AlgorithmKristine Monforte Coma UritaNo ratings yet
- 3 Combined AHA BLS ACLS Updates CombinedDocument5 pages3 Combined AHA BLS ACLS Updates Combinedamanrup randhawa100% (1)
- Emergency Medical Procedures GuideDocument57 pagesEmergency Medical Procedures GuideDuane Liloc100% (1)
- ACLS Provider Manual Supplementary MaterialDocument86 pagesACLS Provider Manual Supplementary MaterialEma0% (2)
- PALS Precourse Self-AssessmentDocument2 pagesPALS Precourse Self-AssessmentGabriel Del RosarioNo ratings yet
- CPR ACLS Study GuideDocument18 pagesCPR ACLS Study GuideJohn Phamacy100% (1)
- Advanced Cardiovascular Life Support (ACLS)Document2 pagesAdvanced Cardiovascular Life Support (ACLS)Vijay MgNo ratings yet
- Topic Discussion Heart Failure MedicationsDocument7 pagesTopic Discussion Heart Failure Medicationsapi-385309917No ratings yet
- 15 Item ACLS Drill With RationaleDocument12 pages15 Item ACLS Drill With RationaleLj Ferolino100% (1)
- CPR Class QuestionnaireDocument4 pagesCPR Class QuestionnaireParikshit PekhaleNo ratings yet
- ACLS Official GuideDocument11 pagesACLS Official GuideICU RSPGNo ratings yet
- Cardiac Arrest Drugs & ProceduresDocument8 pagesCardiac Arrest Drugs & ProceduresAstri Adel BudiarsoNo ratings yet
- Acls Book PDFDocument63 pagesAcls Book PDFSabir Khan67% (3)
- EKG Rhythms: SVT, Atrial Fibrillation, AV Blocks (39Document10 pagesEKG Rhythms: SVT, Atrial Fibrillation, AV Blocks (39Saidel ElizondoNo ratings yet
- ACLS DrugsDocument4 pagesACLS DrugsEduard Espeso Chiong-Gandul Jr.No ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Registered Professional Nurse: Passbooks Study GuideFrom EverandRegistered Professional Nurse: Passbooks Study GuideNo ratings yet
- Cormie2011 PDFDocument22 pagesCormie2011 PDFGust AvoNo ratings yet
- Dental and anesthesia procedures and equipmentDocument56 pagesDental and anesthesia procedures and equipmentVijay RanaNo ratings yet
- Fluid and Electrolyte Therapy in NewbornsDocument10 pagesFluid and Electrolyte Therapy in NewbornsJaner BanosNo ratings yet
- Cileni Cortes Camacho AntologiaDocument62 pagesCileni Cortes Camacho AntologiaCileni CortesNo ratings yet
- PB - Interpreting An Investigation of Plant Hormones QPDocument6 pagesPB - Interpreting An Investigation of Plant Hormones QPRutba SafdarNo ratings yet
- Blood Supply of BrainDocument49 pagesBlood Supply of BrainDarling Sevenfoldism SynysterNo ratings yet
- Respiratory SystemDocument26 pagesRespiratory SystemYasser AhmedNo ratings yet
- CSOM of Middle Ear Part 2Document55 pagesCSOM of Middle Ear Part 2Anindya NandiNo ratings yet
- Classification and Types of StrokeDocument11 pagesClassification and Types of StrokeJose Enrique OrtizNo ratings yet
- Jeffrey SatinoverDocument7 pagesJeffrey SatinoverlooiiiiisNo ratings yet
- Sleep & Traumatic Brain InjuryDocument3 pagesSleep & Traumatic Brain Injury彭金辉 KIVINo ratings yet
- The Progressive Muscle RelaxationDocument4 pagesThe Progressive Muscle Relaxationmaier_gabriela943980% (5)
- Animal Vision EssayDocument6 pagesAnimal Vision EssayFarrah ZainolNo ratings yet
- Investigation of Plasma Protein DisordersDocument10 pagesInvestigation of Plasma Protein DisordersJosiah BimabamNo ratings yet
- Interoception-201 March-2019Document38 pagesInteroception-201 March-2019api-526165635No ratings yet
- Abdominals: Ab Crunch MachineDocument24 pagesAbdominals: Ab Crunch Machinearies_02No ratings yet
- NO Nama Alat Jumlah Kondisi Baik RusakDocument6 pagesNO Nama Alat Jumlah Kondisi Baik RusakRumah Sakit Umum KartiniNo ratings yet
- Cranial NervesDocument118 pagesCranial NervesGan'sNo ratings yet
- Understanding CLL: A Guide For Patients Who Want To Take Charge of Chronic Lymphocytic LeukemiaDocument4 pagesUnderstanding CLL: A Guide For Patients Who Want To Take Charge of Chronic Lymphocytic LeukemiaNakul Singh ParkwayIndiaNo ratings yet
- Psychology: Motivation and EmotionDocument45 pagesPsychology: Motivation and EmotionAisyah AzmiNo ratings yet
- B2.1 Membranes and Membrane Transport [SL_HL]Document39 pagesB2.1 Membranes and Membrane Transport [SL_HL]taleenwas2No ratings yet
- LingalaDocument4 pagesLingalaFabio Ando Filho0% (1)
- 18 Tricks To Teach Your BodyDocument4 pages18 Tricks To Teach Your BodyigiNo ratings yet
- CARDIOVASCULAR - SYSTEM Group No.3 MODULEDocument12 pagesCARDIOVASCULAR - SYSTEM Group No.3 MODULEDavid Paul LanuzaNo ratings yet
- 01 - Newborn Physical ExamDocument2 pages01 - Newborn Physical Examgerald_valeriano0% (1)
- LP Surgery ChestDocument6 pagesLP Surgery Chestangelmd83No ratings yet
- How Your Diet Affects Your BrainDocument2 pagesHow Your Diet Affects Your BrainRusso Dalmasso50% (2)
- Cellular ComponentsDocument2 pagesCellular ComponentsWangSheng TanNo ratings yet
- The Problem and Its BackgroundDocument43 pagesThe Problem and Its BackgroundkjjkjkljkjjklNo ratings yet
- CH 11 AnswersDocument23 pagesCH 11 AnswersJennifer Bash100% (4)














































































![B2.1 Membranes and Membrane Transport [SL_HL]](https://imgv2-2-f.scribdassets.com/img/document/720749257/149x198/1c59214fd9/1712460993?v=1)








