Professional Documents
Culture Documents
Intensive Care Management of The Head Injured Patient: Review Article
Uploaded by
rickyGKOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intensive Care Management of The Head Injured Patient: Review Article
Uploaded by
rickyGKCopyright:
Available Formats
Indian Journal of Neurotrauma (IJNT)
81
Review Article
2006, Vol. 3, No. 2, pp. 81-94
Intensive care management of the head injured patient
V. Bhadri Narayan, MD
Associate Professor
Department of Neuroanaesthesia, NIMHANS, Bangalore
Abstract : Traumatic brain injury is a significant cause of mortality and morbidity in patients below
the age of 40 years, and is a socio-economic burden on the society. Patients with severe head injury
require comprehensive care preoperatively, intraoperatively and postoperatively. The aim would be
to prevent secondary brain injury by maintaining cerebral perfusion pressure, intracranial pressure
and cerebral blood flow. Head injury is often associated with intracranial and extracranial
complications. Timely diagnosis and correction of these complications will improve outcome in these
patients.
Keywords: brain injury, cerebral perfusion pressure, cerebral blood flow, monitoring, intracranial
pressure
INTRODUCTION has been proposed in dealing with risk-taking behaviors
and substance abuse. The basic premise is that a patient
Traumatic brain injury is a major cause of death, who has suffered an injury event may be more open to
disability and is a serious socio-economic problem. The counseling on safe behaviors, and more willing to change
mortality in patients with brain injury is unacceptably behaviors, if approached in the emergency setting.
high between 35-50 % and over the last few decades the Further research is needed to assess what methods are
mortality has shown a decrease of about 10% per decade. most effective at changing risky behaviors. Seatbelt use
This has been possible because of improved in automobiles and helmet use by motorcyclists and
understanding of the pathophysiology, new modalities bicyclists have also been demonstrated to be effective
of monitoring and therapeutic strategies. However, ways of reducing TBI but are not in universal practice,
despite enormous efforts and huge investments the search and should be implemented to reduce the incidence of
for the magic bullet for cerebral protection is still elusive. head injuries3,4.
As we understand the complex pathophysiology following
head injury it is unlikely that such a magic bullet will Physiological Alterations
ever be found. The strategy that is most likely to help in The injured brain itself has systemic effects on physiology
the management will be a pharmacologic cocktail aimed and homeostasis that may result in secondary injury. A
at the multiple pathomechanisms. posttraumatic sympathetically mediated catecholamine
The role of prevention release may result in a hyperdynamic cardiovascular
response that may lead to any of three clinical complexes:
Emergency physicians can have an important role in the severe neurogenic hypertension, cardiac dysrhythmias,
prevention of TBI by promoting safety legislation, and myocardial ischemia.5. The hyperdynamic response
designing prevention programs, and serving as educators in the patient with severe TBI is typically characterized
and teachers. One example of a prevention program, by sustained, severe hypertension, with an associated
called THINK FIRST, has been developed by increase in cardiac index and heart rate and a normal to
neurosurgical associations. This program teaches school- decreased systemic vascular resistance. The patient may
age children behavioral and preventive measures to be relatively hypervolemic, even with a normal
reduce the risk of head injury and spinal cord injury1. pulmonary capillary wedge pressure. There is typically
Early evaluations of this program suggest that it may be an associated increase in urine output. There may be an
effective in changing risk-taking behavior2. In terms of increase in plasma epinephrine and norepinephrine levels.
emergency practice, the concept of a “teachable moment” Electrocardiographic findings may include a prolonged
QT interval (in 89% of patients), U waves, peaked T
Corresponding author:
Dr Bhadri Narayan, MD
waves, and premature atrial contractions. Subendocardial
Department of Neuroanaesthesia hemorrhages have been documented in 50% of autopsied
NIMHANS, Bangalore-560029 patients.
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
82 V. Bhadri Narayan
Pulmonary effects appear in two varieties. The most of head injured patients. Blunt brain injury activates the
common effect, occurring in over 85% of severe TBI coagulation process, and in two thirds of TBI patients
patients, is that of neurogenic hypoxia. This is manifested results in parameters suggestive of disseminated
as an increase in the alveolar-arterial oxygen intravascular coagulation (DIC) (i.e., elevated D-Dimer,
concentration gradient without a radiographic decreased fibrinogen, increased PT and PTT). Patients
abnormality. It may last a few days in survivors but tend to demonstrate a two-phase coagulopathy. In the
persists in nonsurvivors. The cause of this ventilation- first 4 hours after injury, a state of relative
perfusion mismatch is unknown but is presumed to be hypercoagulability mediated by plasmin and thrombin
related to hypothalamic dysfunction or microatelectasis. develops; by 4 hours posttrauma, coagulation pathway
A rarer but more obvious pulmonary effect of severe substrates are exhausted and a subsequent stage of
brain injury, typically associated with the most severe consumptive coagulopathy ensues. The degree of
injuries, is neurogenic pulmonary edema. This classically posttraumatic perturbation in the prothrombin time (PT),
has an immediate onset and becomes clinically evident platelet count, thrombin clotting time (TCT), and
as dyspnea, tachypnea, hypoxemia, and “fluffy” infiltrates especially the APTT has a strong association with
on chest x-ray from 2 to 12 hours after injury. It is mortality. Patients with coagulopathy are nine times more
typically a transient, self-limited process lasting hours to likely to die, and commonly demonstrate an interval
days. The etiology is relatively undefined, but may result progression of injury or development of new lesions on
from increased pulmonary intravascular pressure caused repeated brain imaging11.
by a catecholamine-mediated decrease in pulmonary
vascular resistance in the setting of a hyperdynamic
PATHOPHYSIOLOGY
increase in cardiac output, or from increased Primary Brain Injury
permeability due to direct endothelial injury6. Pulmonary
The underlying pathophysiology of TBI can be divided
vascular endothelial and parenchymal damage could
into primary and secondary events. Primary brain injury
theoretically result from the cytokine release that follows
results directly from the disruptive mechanical forces
TBI7. Depletion of lung surfactant and pulmonary
imparted to the brain during the traumatic event.
microembolism may also play a role. Other pulmonary
Manifestations of such injury can be either focal or
complications of severe TBI include aspiration, infection,
diffuse. Focal injury includes cerebral contusions,
and pulmonary embolus.
intracerebral hematomas, epidural hematomas, subdural
Electrolyte abnormalities can result from severe TBI. hematomas, or subarachnoid hemorrhage12. Diffuse
Hyponatremia, either from the release of antidiuretic primary brain injury may result from the shear forces
hormone, the syndrome of inappropriate secretion of generated by trauma and is manifested as diffuse axonal
antidiuretic hormone (SIADH), or, uncommonly, injury (DAI)13. Axonal injury is common in TBI and
cerebral salt wasting, is the most common electrolyte appears to account for much of its morbidity14.
abnormality following TBI. SIADH is associated with
hyponatremia, serum hypo-osmolarity, and urine
Secondary Brain Injury
hyperosmolarity. Diabetes insipidus, which occurs in Neurochemical events: Secondary brain injury results
less than 1% of TBI patients, may result in hypernatremia, from physiological processes and neurochemical
with an associated serum hyperosmolarity and urine cascades, either triggered by or associated with the
hypo-osmolarity. primary injury, that continue after the initial traumatic
event. Delayed axonal injury may occur 4 to 24 hours
Perhaps the most insidious abnormality after TBI is
after the initial injury and is thought to involve secondary
coagulopathy. Parenchymal disruption of brain tissue is
calcium-mediated proteolytic processes that compromise
known to activate the coagulation system, presumably
the axonal cytoskeleton15. The accumulation of delayed
from activation of the extrinsic pathway by tissue
secondary axotomies appears to constitute a more
thromboplastin8. An abnormal level of fibrin degradation
prominent injury process than that from primary
products (FDP) has been found to be the most prevalent
axotomies. Histological studies on experimentally injured
abnormality, in one study occurring in all patients with
animals, corroborated by postmortem histological studies
severe TBI.9,10. An elevation of the activated partial
on humans, reveal a process that starts with a focal
thromboplastin time (APTT) can be found in over 25%
impairment of anterograde axonal transport followed by
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
Intensive Care Management of the Head Injured Patient 83
axonal swelling and disconnection, and then formation for other types of critically ill patients.
of axonal retraction balls16.
Nutritional Assessment
Somatic neuronal injury is mediated in part by the
Body weight: Though seemingly straight-forward, body
release of excitatory amino acid neurotransmitters,
weights in ICU are difficult to measure as they are often
which leads to widespread neuronal depolarization,
distorted by changing fluid distribution. Consequently,
followed by massive calcium ion influx through voltage-
the patient’s current weight should be compared with
sensitive channels such as the N-methyl-D-aspartate
his/her usual or ideal body weight. A weight loss
(NMDA) receptor complex. Free-radical generation and
exceeding 10% signifies that the patient is at high risk
lipid peroxidation result in neuronal membrane
of malnutrition. Devices are available which will measure
deterioration and subsequent cell lysis. Other injurious
body weight daily in ICU.
biochemical cascades, involving agents such as nitric oxide
and cytokines, result in further and delayed damage, with Anthropometric measurements: Mid-arm circumference
subsequent brain swelling and edema17,18,19. and triceps skin fold thickness can be used but are not
reliable in the ICU as they can get obscured by severe
The cranial vault is a fixed space containing three
edema and nutritional deficiencies.
compartments: brain tissue, cerebrospinal fluid (CSF),
and blood (intravascular volume). As posttraumatic brain Laboratory tests: A number of biochemical investigations
swelling ensues, the CSF and vascular compartments are can guide the state of preexisting nutrition in patients.
less and less able to compensate through the relative The levels of albumin, prealbumin and transferrin will
extrusion of their respective components, and intracranial normally give a balanced view of patient status but are
pressure (ICP) begins to rise sharply20. This can lead to less reliable in the ICU during periods of critical illness
regional ischemia and herniation. Increased ICP (over resulting from aggressive fluid resuscitation. Prolonged
20 mmHg) has significant adverse effects on outcome stays in the ICU also can change these values. The total
and survival from severe TBI 21,22,23. leukocyte count gives a reliable indicator of the
immunological status of the patient, which indirectly
MANAGEMENT IN THE ICU reflects the nutritional status.
Nutrition: Nutritional assessment of the critically ill
Body mass index: This is more optimal indicator of
patient is crucial as deterioration in nutritional status
nutrition. BMI is given by body weight in kilograms
can have a profound effect on the outcome. The route,
divided by squares of the height in metres. BMI The
manner, adequacy of nutritional support affects the
Harris-Benedict equation provides a satisfactory method
degree of stress response, incidence of nosocomial
to develop an initial estimate of basal energy expenditure
infections/ multiorgan failure, length of hospitalization,
(BEE) based on weight and gender. BMI values for women
morbidity and mortality. While short periods of starvation
are 1-22.4, 2-26.9, 3-31.4 and for men 1-22.7, 2-27.2,
over hours or a day or two may not be detrimental for
2-31.8; 1 is normal and 2 and 3 are over weight.
most patients, the difficulty of maintaining or increasing
lean body mass during critical illness is too great to delay Goals of nutritional support
instituting artificial feeding long, even if the patient is
The fundamental goal of nutritional support for the
well nourished at the outset.
critically ill head-injured patient is to provide protein
Although the brain does not participate in mechanical and calories in amounts sufficient to match the demands
work, osmotic work, or extensive biosynthesis, processes of hypermetabolism and increased protein breakdown.
which use quite large amounts of energy. Nutritional In addition, it is important to provide adequate
management in some patients can be an essential factor micronutrients in order to meet the increased demand
necessary for survival. After the initial neurologic insult imposed by stress. Full nutritional support is generally
the incidence of death from extracranial causes such as not initiated immediately after injury. Reasons for the
sepsis increases dramatically 23 . Bodily defense delay include the time required for accurate assessment,
mechanisms against such secondary insults as septicemia, the need for resuscitation and/or early trauma care, and
pneumonia, and meningitis rely heavily on adequate the potential complicating metabolic effects of aggressive
nutritional support24. Assessment of nutritional needs in feeding during the early, unstable period. Virtually all
the neuro-ICU patient is similar to methods employed severely injured patients, therefore, experience a period
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
84 V. Bhadri Narayan
of temporary starvation. Nutritional support should, feeds, are much less expensive and may minimise
however, be started as soon as possible after injury and intestinal mucosal atrophy, bacterial translocation and
should be maintained as long as the patient does not eat endotoxinemia. Lack of bowel sounds alone is not a
adequately25. Support can almost always be initiated reason to withhold enteral feeding and does not correlate
within 2 to 4 days after the injury. The current approach well with rates of gastric emptying.
to nutritional support of the critically ill head injured
patient is to provide a broad array of the macronutrients Calories/Energy Needs
and micronutrients that are necessary for health. If Overall caloric assessment in TBI patients is determined
catabolic illness alters the requirements for specific by the Harris-Benedict equation, which provides a
nutrients, then the administration of required substrates satisfactory method to develop an initial estimate of basal
might facilitate a patient’s anabolic response to a life- energy expenditure (BEE) based on weight and gender.
threatening illness26. Enteral nutrition is the preferred
route of nutrient administration in the critically ill head BEE(men)= 66.47 + 13.75W + 5.00H – 6.76A
injured patient. It maintains the integrity of gut mucosa BEE(women)= 655.10 + 9.56W + 1.85H – 4.68A
and has immunologic advantages over parenteral
(W=weight in kg, H=height in cm, A=age in years)
nutrition. Because it is usually not possible to start enteral
nutrition immediately in the critically ill or injured Indirect calorimetry
patient, parenteral nutrition is an important therapeutic
Whenver possible, because indirect calorimetry
modality. Patients who cannot tolerate full enteral
quantifies oxygen conumption and CO2 production as
nutrition may be managed with parenteral nutrition alone
determinants of energy use, which helps prevent under-
or with combination feeding, a modality in which
and over-feeding of patients. Short-term second hourly
parenteral nutrition is gradually tapered off as the enteral
indirect calorimetry reliably reflects 24-hour metabolic
formula’s use is advanced.
utilization in clinically stable, sedated, ventilated patients.
Hypermetabolism, an accelerated catabolic rate and Metabolic rate of patients with temperature fluctuations
rampant nitrogen losses are consistent sequelae to major may vary as much as 25% in the course of a day and
trauma, particularly acute traumatic brain injury and benefit from ongoing measurement. Calories can be
acute spinal cord injury (ASCI). A well-documented estimated at 35 to 40 kcal/kg/d to account for the large
hypermetabolic, catabolic injury cascade is initiated increase in metabolic rate. Monitoring for hyperglycemia
immediately after central nervous system injury that is necessary to prevent adverse effects.
results in depletion of whole-body energy stores, loss of
Protein needs in TBI patients
lean muscle mass, reduced protein synthesis, and
ultimately, loss of gastrointestinal mucosal integrity and Protein requirement in TBI patients is estimated at 1.5
compromise of immune competence. Severely brain- – 2.2 g/kg of body weight. Non-supplemented TBI
injured and spinal cord injury (SCI) patients, therefore, patients can lose up to 10% of lean body mass in a week,
are at risk for prolonged nitrogen losses and advanced up to 25% in two weeks and 30-40% in three weeks.
malnutrition within 2 to 3 weeks after injury with Negative nitrogen balance is determined by estimating
resultant increased susceptibility for infection, impaired nitrogen losses, which can be as high as 30 g/day in
wound healing and difficulty in weaning from mechanical acute TBI patients. Negative nitrogen balance usually
ventilation. persists for 2-3 weeks, regardless of the protein provided,
with a peak at about 10 days post-injury. The amount of
The basic aim is to provide an optimal environment nitrogen loss correlates with serum levels of epinephrine,
for survival and repair of the damaged neuronal pool. norepinephrine, glucagons and hormones associated with
While short periods of starvation over hours or a day or hypermetabolism. The hypermetabolic response and the
two may not be detrimental to most of the patients, the release of hormones correlated with the severity of injury.
difficulty of maintaining or increasing lean body mass Immobility may potentiate nitrogen losses, as does
during critical illness is too great to delay instituting steroid administration during the first six days post-injury.
artificial feeding long, even if the patient is well nourished Provisionof more protein than 1.5 to 2.2 mg/kg of body
at the outset. The route should be enteral when possible. weight results in heightened nitrogen excretion.
Enteral feeds tend to be more complete than parenteral
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
Intensive Care Management of the Head Injured Patient 85
Amino acid patterns in TBI patients feeding in head injured patient has been shown to
increase the mortality 30. Enteral feeding following
There are large fluxes in alanine and glutamine, which
neurosurgical procedures was associated with accelerated
demonstrate skeletal muscle protein release lower levels
normalized nutritional status and improved substrate
of leucine, isoleucine and valine and high levels of
tolerance31. Enteral nutrition is equivalent or superior
phenylalanine.
to parenteral nutrition in patients with head injuries.
Vitamins, mineral and fluid patterns in TBI Early enteral feeding has established benefits over feeding
patients later in course of hospitalization. Patients with TBI are
candidates for parenteral nutrition when they cannot
There are decreased plasma levels of many B vitamins tolerate enteral nutrition because of ileus or a high risk
and vitamin C, increased urinary zinc excretion/low of aspiration. The recommendation at present is to
serum zinc levels and salt wasting in some patients. provide 30-35Kcal/kg: 60% of the caloric requirement
Phosphorus, potassium and magnesium decreases in is with carbohydrates, 15-20% as proteins at 1.5 -2gms
some patients with the initiation of feeding. of proteins /kg and the remainder as fats. The
Supplementation with vitamins and minerals is complications of enteral therapy are overfeeding,
recommended if the nutrition regimen falls below the azotemia, fat overload syndrome, hypertriglyceridemia,
recommended dietary allowances (RDA). hepatic steatosis, hypercapnia, metabolic acidosis,
Lipids diarrhea, refeeding syndrome, central line
complications32.
It is essential to provide a lipid source with 50-70%
medium chain triglycerides and an omega-3 ratio of Refeeding syndrome
2:1 to 8:1 27. A minimum of 10% of the caloric Initiation of nutritional support to patients with severely
requirement must be in the form of lipids to prevent depleted nutrient stores is associated with clinically shifts
essential fatty acid deficiency. Care should be taken to in phosphorus, magnesium and potassium from
ensure that excessive lipids are not administered, as it extracellular to intracellular space 33 . Additionally,
can cause immunosuppression. If triglyceride levels starvation causes a catabolic release of intracellular
become more than 300 mg, then the lipids will have to phosphate which is excreted in urine. The total body
be reduced. stores of intracellular electrolytes are slowly depleted.
The initial caloric estimate is adjusted based on the Refeeding and the early stages of over feeding are both
qualitative assessment of factors altering the need. Head demanding on the cardiovascular system. Patients who
trauma patients have a 1.5 to two-fold increase in the are chronically malnourished have depletion in cardiac
metabolic needs associated with a massive nitrogen loss. muscle, and are unable to meet circulatory demands
There is debate about optimal inputs of nitrogen in the imposed by aggressive nutritional support. Approaches
context of the short- to medium-term artificial feeding to prevention of refeeding syndrome are to slowly
in trauma, sepsis and critical illness, and no outcome introduce nutritional support and at the same time allow
trials allow resolution of the argument. Emphasis has for the addition of vitamins, zinc and other minerals.
been traditionally placed on the maintenance of zero or Refeeding syndrome carries considerable morbidity and
positive nitrogen balance and numerous studies examine mortality34.
optimal inputs under various clinical conditions. Some Guideline for Closed Head Injury patients :
show improving balance with increasing input to levels
of 364 mg N/kg per day28 in depleted patients or 400 mg Fever and sepsis increases calorie requirement by 7.2%
N/kg per day in patients who were described as well for every degree Fahrenheit above normal temperature.
nourished or minimally undernourished27. Patients with Seizures and extensor posturing increases calorie
GCS of 4-5 have the highest energy expenditure. Patients requierement by 20-30% to a maximum of 3500-4000
who are brain dead or who are receiving sedatives, calories (total). Non-sedated coma increases BEE by
barbiturates or musculoskeletal blocking agents have an 140%, while pentobarbital coma increases BEE by 100-
average of 14% lower energy expenditure. 120%. Standard TBI range is 140-200% BEE. Calories
are therefore supplied at 40-70% above basal needs, with
Feeding should be started as early as possible as non 30-40% as lipids to minimize hyperglycemia based in
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
86 V. Bhadri Narayan
part on the patient’s GCS and MREE (measured resting disadvantages. The rationale for sedation are multifaceted
energy expenditure). include analgesia, anxiety, agitation control, reduction
of the stress response and adaptation to ventilatory
Deep Vein Thrombosis Prophylaxis support43.
Thromboembolic phenomena continue to be a significant
Problems of under sedation are increased stress
cause of morbidity and mortality in neurosurgical
symptoms such as hypermetabolism, sodium and water
patients. Deep vein thrombosis formation is encouraged
retention, lipolysis, cardiovascular symptoms like
by a number of clinical situations. A number of
tachycardia, increased blood pressure, increased oxygen
predisposing factors have been identified which can
consumption, altered respiratory rates and changes in
promote deep vein thrombosis such as recent surgery,
coagulation parameters. On the other hand over-sedation
malignancy, immobilization, trauma, acute stroke,
also carries risks like increased venous thrombosis,
pregnancy, antithrombin , protein C and protein S
decreased blood pressure, increased stay in the ICU and
deficiency . Many of these factors coexist in
prolonged use may result in withdrawal symptoms44.
neurosurgical patients, which puts them in the high risk
category for the development of deep vein thrombosis35. There are a number of agents available for use in
The primary concern is the potential for pulmonary clinical practice .The most commonly used drugs are
embolism. morphine, pethidine, fentanyl, midazolam, propofol,
lorezapam and recently the µ2 agonist dexmedetomidine
Methods to prevent DVT include the use of
has been found to be a very useful agent and may play a
intermittent pneumatic compression, elastic compression
major role in the management of patients in the future.
stockings, early ambulation, physical therapy and low
dose anticoagulation. These methods have been found Intracranial Pressure and Cerebral perfusion
to effectively prevent DVT. In neurologic or pressure
neurosurgical patients there is concern that
anticoagulation may predispose these patients to The intracranial pressure is elevated in 50-75 % of
intracranial hemorrhage though there is no evidence to patients with severe head injury who remain comatose
support this36. Recently perioperative minidose heparin after resuscitation. ICP (Intracranial pressure) is more
has been found to be safe in patients undergoing than 20 mm Hg during the first 24 hours and generally
craniotomy for supratentorial tumors37. comes down within 48 hours. In the severely brain
injured patient, signs of increased ICP include a change
Gastric Ulcer Prophylaxis or asymmetry in pupillary reactivity to light or a new
eccentricity in one of the pupils. A dilated unreactive
Stress ulcers occur frequently in intensive care unit (ICU)
pupil and Cushings triad of hypertension, bradycardia,
patients who have intracranial disease. After major
and irregular respirations are late signs45. This incidence
physiological stress such as brain injury, endoscopic
of elevated ICP approaches 60% if at least two of the
evidence of mucosal lesions can appear within 24 hours,
following risk factors are present: (1) age over 40 years;
and 17% of these erosions can progress to clinically
(2) SBP less than or equal to 90 mmHg; and (3) unilateral
significant bleeding38. Gastrointestinal (GI) hemorrhage
or bilateral motor posturing, either flexor or extensor46.
has been associated with mortality rates of up to 50%
39,40,41,42 It is therefore recommended that ICP monitoring be
. The pathogenesis of stress ulcers may not be
instituted for all severe TBI patients with abnormality
completely understood, but gastric acid and pepsin
on head CT and for all severely brain injured patients
appear to play significant roles.
with a normal head CT but two or more of the risk
Sedation and Analgesia factors mentioned. Normal ICP in humans is between
0 and 10 mmHg. Eisenberg et al noted that patients
Sedation is a fundamental element in the intensive care
whose ICP could be controlled with pentobarbital had a
unit, but maybe problematic in the neuroICU as it could
better outcome than those in whom ICP could not be
make assessment difficult. The primary aim of the
controlled; 92% of those who responded to ICP reduction
neurointensive care is to maintain cerebral perfusion
therapies survived, whereas 83% of those who did not
pressure, reduce intracranial pressure and cerebral
respond died47. A widely accepted treatment threshold
metabolic requirement. There are different
is an ICP above 20 mmHg sustained for over 10 minutes.
pharmacologic agents available each with advantages and
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
Intensive Care Management of the Head Injured Patient 87
Studies have shown that as the ICP increases the mortality hypertension, arrhythmias, acute myocardial infarction
also increases48. and pulmonary edema. Hypotension is one of the most
important factors and is an independent predictor of
The major cause of raised ICP, apart from hematomas outcome. A single episode of hypotension increases
is brain swelling. The factors responsible for post- mortality two fold49,50. The maintenance of cerebral
traumatic brain swelling are not clear, however there is perfusion pressure (CPP) is crucial in the prevention of
convincing evidence for both cytotoxic and ischemic - cerebral ischemia. There is a correlation between CPP
hypoxic influences. The goal will be to control ICP, and outcome that is stronger than that of
provide adequate cerebral perfusion pressure (CPP),
oxygenation and to prevent herniation. The CPP should ICP and outcome. A CPP of less than 60 mmHg for
be maintained greater than 70mm Hg. Treatment should over 33% of the time is strongly associated with death,
be based on knowledge of regional cerebral blood flow whereas a CPP of greater than 90 mmHg is associated
(rCBF) metabolism and function. ICP and CPP can be with a 75% incidence of good outcome51. Maintaining
measured easily and provide the best indirect a CPP of greater than 70 mmHg, even with induced
measurements of tissue perfusion. Advance monitoring hypertension, is associated with significant
technology like Jugular venous oxygen saturation (SjVO2), improvements in the morbidity, mortality, and outcome
Brain tissue oxygen tension (PbtO 2), Transcranial of severe TBI patients when compared with management
Doppler (TCD), Near Infrared Spectroscopy (NIRS), using ICP control alone52.
evoked potentials and intracerebral microdialysis Pressor therapy is begun with the presumption that
provides the information on both regional and global any deficits in intravascular volume have been adequately
cerebral blood and metabolism and will probably guide corrected. Agents that have been used successfully
therapy of the head injured patient in the future. Table include norepinephrine (4 mg/250 mL 0.9% NaCl) to a
1 shows cerebral and systemic characteristics of various maximum dose of 0.4 micrograms/kg per minute and
pharmacological agents used in head injury for cerebral phenylephrine (40 to 80 mg/250 mL 0.9% NaCl) to a
protection. maximum dose of 4.0 µg/kg per minute. Dopamine (400
Cardiovascular Management mg in 250 mL of 0.9% NaCl), at 1.5 to 3.0 µg/kg per
minute, should be added for renal protection. The
The major goals in the management of the patient with minimum vasopressor dose necessary to augment CPP
head injuries is to prevent and treat hypotension, to an efficacious level should be used, keeping in mind
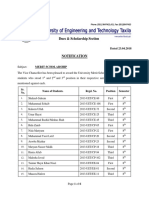
Table 1: Cerebral and systemic characteristics of pharmacological agents
Propofol Midazolam Lorazepam Fentanyl Remifentanil
Rapid onset +++ +++ + +++ +++
Fast recovery +++ ++ + ++ +++
Easily titrated +++ ++ + ++ +++
ICP reduction ↓↓ ↓ ↓ ↓/↔ ↓/↔
CBF reduction ↓↓ ↓↓ ↓ ↔ ↔
CMRO2 reduction ↓↓ ↓ ↓ ↓ ↓
MAP ↓↓ ↓ ↓ ↓ ↓
↔ no clear effect , ↓ modest decrease , ↓↓ pronounced decrease , +++ very favorable , ++ favorable +
not favorable , CBF –cerebral blood flow , CMRO2 cerebral metabolic rate of oxygen , ICP intracranial
pressure , MAP mean arterial pressure
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
88 V. Bhadri Narayan
that a supranormal CPP (e.g., 80 to 90 mmHg) may be catecholamine release with adequate sedation and beta
necessary. At the same time, a CPP greater than 113 blockers maybe able to prevent or ameliorate myocardial
mmHg may result in a reversal of therapeutic effect53,54. injury58. It has been suggested that electrocardiographic
changes seen following head injury may indicate a more
Hypertension severe head injury and thus carry a higher mortality59.
Blood pressure management in a important issue in the
Neurogenic Pulmonary Oedema
neurointensive care unit. Concern arises that systemic
hypertension may exacerbate cerebral edema, intracranial This is one of the most dramatic sympathetically
hemorrhage and have deleterious cardiopulmonary mediated processes. It follows a profound sympathetic
effects such as pulmonary edema and myocardial discharge which leads to a redistribution of blood from
ischemia. Conversely a decrease in blood pressure may the systemic to the pulmonary vasculature resulting in a
lead to insufficient perfusion and it has been well rapid rise in pulmonary pressures60. ther mechanisms
documented that the drop in pressure may be a that may be involved are neurogenic depletion of
forerunner for the genesis of plateau waves. Neurogenic pulmonary surfactant61. Typically neurogenic pulmonary
hypertension is common following head injury and oedema is self limiting. Treatment is primarily supportive
appears to be sympathetically mediated and is directly and is aimed at ensuring oxygenation with mechanical
proportional to the catecholamine release. Increased ICP, ventilation and positive end expiratory pressure.
brain stem compression and medullary ischemia may
be associated with severe hypertension 55. When or Respiratory Care
whether to treat hypertension is controversial. An The goal of mechanical ventilation in patients with brain
elevated systemic arterial pressure may be an intrinsic injury is to optimize blood gas exchange and minimizing
compensatory mechanism for impaired cerebrovascular the intrathoracic pressure. The goals to achieve are a:
autoregulation and low perfusion pressure. Lowering PaO2 >90 mm Hg and PaCO2 between 35 and 45 mm
arterial pressure to normal levels may lead to ischemia, Hg. How these goals can be achieved is still matter of
cellular hypoxia and cerebral edema56. controversy. The use of normal tidal volume (VT) and
low positive end expiratory pressure (PEEP) level is
Blood pressure should be treated when the pressure
suggested as the “gold standard” ventilatory strategy after
exceeds 180/110 mm Hg or a mean greater than 150
acute brain injury. This accomplishes cerebral
mm Hg. The choice of antihypertensive agent is not
hemodynamic requirements: mild hyperventilation to
straightforward. Therapeutic urgency, brain protective
control intracranial pressure (ICP), minimizing
effect and the potential to increase ICP are all important
intrathoracic pressure to reduce interference with
considerations in the choice of the drug. In the face of
cerebral venous drainage. On the other hand, there is
an elevated ICP beta blockers are the preferred drugs57.
evidence that the use of high VT with low level of PEEP
Arrhythmias can induce and exacerbate acute lung injury62.63. Therefore
the ventilatory management of patients with acute severe
A wide range of cardiac arrhythmias may occur as a
brain injury remains a challenge for clinicians.
result of centrally mediated sympathetic and vagal
discharge. Tachyarrhythmias are predominantly Airway Management
supraventricular and include atrial fibrillation, flutter and
Patients with acute severe brain injury are unable to
paroxysmal atrial tachycardia. Ventricular
protect their airways and should therefore be intubated.
tachyarrhythmias are uncommon. Nodal and sinus
The technique of intubating patients will depend on
bradycardia are associated with sustained intracranial
cervical spine (C-spine) clearance. It is imperative that
hypertension and rarely require treatment.
C-spine injury is ruled out as early as possible. Those
Myocardial Injury involved in managing the airway of patients with
confirmed or potential C-spine injury must be aware of
Myocardial injury in the absence of coronary artery
the advantages and disadvantages of the possible
disease is seen in upto 50% of head injured patients.
techniques so that the safest one is chosen for the patient.
The changes observed are similar to those found after
Patients with injuries above the calvicles are at increased
myocardial infarction, subarachnoid haemorrhage and
risk, and this risk is increased 4-fold64, if there is clinically
prolonged catecholamine therapy. Inhibition of
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
Intensive Care Management of the Head Injured Patient 89
significant head injury (GCS<9). Cervical spine injury and ICP in head-injured patients. Evidence is
is often occult, and present in upto 20% of patients with accumulating that this may not be the case, especially in
head injuries and hence secondary injury to the spinal hypotensive patients. Ketamine is a non-competetive
cord must be avoided. Patients with acute severe brain NMDA receptor antagonist and has been shown to have
injury are unable to protect their airways and should neuroprotective effects.
therefore be intubated. The techniaue of intubating
patients will depend on C-spine clearance. It is prudent Failed Intubation
to have C-spine clearance to prevent untoward incidents. Failed or difficult intubation is always a problem. It is
C-spine clearance in a conscious individual is dependable important to preoxygenate patients before attempted
based on clinical signs described. The five criteria are intubation to avoid desaturation while making repeated
no posterior cervical midline tenderness, alert patient, attempts at intubation. Alternative methods of securing
no focal neurological deficits, no intoxication and no the airway should be instituted as soon as a problem is
painful distracting injuries 65. Criteria for C-spine recognized. The methods that are available to secure
clearance are more controversial in the unconscious the airway are the laryngeal mask airway (LMA),
patient. In the unconscious patient the recommendation combitube, cricothyrotomy and emergency
is to have three views of C-spine radiograph: anterior- tracheostomy if trained hands are available.
posterior, lateral and open mouth views to rule out C-
spine injury. If C-spine is not cleared, intubation is Two aspects of airway management that are prominent
attempted as if a C-spine injury is present. Direct in the ICU are the decisions regarding oral versus nasal
laryngoscopy has been shown to disturb the cervical spine intubation and timing of tracheostomy. Orotracheal
both in anesthetized volunteers and in cadavers66,67. intubation is the fastest and surest method of intubating
Manual axial in-line neck stabilization reduces this the trachea. Oral intubation is preferred particularly if
movement by 60%. Atlantooccipital extension is basilar skull fractures are present. Nasotracheal
necessary to bring the vocal cords within line-of sight of intubation is contraindicated in patients with potential
the mouth. Thus, patients with unstable C1 or C2 injuries base of skull fractures or unstable mid-face injuries. In
might be at more risk from this technique. The addition, it may produce hemorrhage in the airway,
commonest site of fractures is at C2, and dislocations making other airway manipulations difficult or
occur commonly at C5/C6 and C6/C7. impossible. Risk factors associated with radiologic
maxillary sinusitis and the incidence of infection among
Patients requiring tracheal intubation should be patients who are critically ill and mechanically ventilated
anesthetized unless they are very cooperative. In the have been determined 68. The four independent risk
obtunded head-injured patient, anesthesia is vital to factors identified were nasal placement of endotracheal
prevent pressor responses to intubation which increases tube, nasal placement of the gastric tube, duration of
intracranial pressure. The ideal intubation agent probably endotracheal tube, and duration of nasogastric tube
does not exist, and is dependent on individual experience. placement. The incidence of maxillary sinus
Thiopentone is very effective and is the standard for abnormalities is upto 75% in the critically ill patients
rapid sequence induction. Propofol is not recommended and oral intubation decreases this complication by 50%.
for trauma because of the potential for hypotension and Acute severely brain injured patients require early
should be used with caution, though its ability to provide endotracheal intubation and may need prolonged
total intravenous analgesia with good control over the mechanical ventilation in the ICU. The timing of
depth of anesthesia may be very valuable. Etomidate has tracheostomy is still controversial. Some studies suggest
been reported to produce less cardiovascular depression that prolonged endotracheal intubation results in
than other intravenous induction agents, but the potential increased glottic and subglottic stenosis, others suggest
adrenal and immunological suppression caused by even that tracheostomy can wait upto five weeks. An ideal
one bolus of etomidate puts a question mark on its use approach would be to assess the patient at the end of
in these patients. Ketamine is very under-used drug which seven days and if the patient is likely to need mechanical
maintains cardiovascular stability better than any of the ventilation further, or have a poor GCS then it is advisable
other intravenous drugs. Its use is currently to do a tracheostomy to optimize airway management
contraindicated in patients at risk from raised intracranial and to prevent post-extubation complications69.
pressure as it is known to increase cerebral blood flow
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
90 V. Bhadri Narayan
Infection Control blood volume in SIADH and a decreased volume in
CSWS. The other difference is a high ADH level in
Fever is common following head injury and is
SIADH and a normal level in CSWS.
documented to worsen outcome70. In addition fever can
raise metabolic requirements, and being a potent Hypernatremia
vasodilator can increase intracranial pressure. Invasive
Diabetes insipidus (DI) is frequent occurrence in the
monitoring in patients with head injuries can predispose
ICU and results from decreased levels of ADH and an
these patients to infection, and should be investigated
inability to concentrate urine. The free water loss causes
with appropriate cultures and antibiotics. The common
hypovolemic hypernatremia. DI is managed by correcting
sources of infection will be from intravascular lines,
the free water deficit with non salt containing solutions
urinary catheters, chest, wound infection and meningitis.
and controlling urinary volume by the administration of
The efficacy of prophylactic antibiotics in patients with
pitressin (vasopressin) 5-10 units subcutaneously ,
traumatic cerebrospinal fistulas is controversial.
desmopressin acetate 2-4 µg intravenously or as a nasal
Antibiotics are recommended only when signs or
spray 2µg73.
symptoms of meningitis develop. Nosocomial infections
are common in neurological and neurosurgical patients Hyperglycemia
with pneumonia, catheter related infection and
meningitis contributing significantly to morbidity and Hyperglycemia has been associated with a poor
mortality. Prevention of infection plays an important role neurological outcome in patients with head injuries74,75.
in reduction of nosocomial infections. The approaches Neurologic damage can be exacerbated when associated
recommended are hand-washing, prevention of cross with secondary insults. TBI is associated with stress
contamination, sterilization and disinfection of medical response that includes hyperglycemia and has been shown
equipment and appropriate use of antibiotics to prevent to worsen neurological outcome during cerebral ischemia
emergence of resistant organisms71. and hypoxia. Patients with severe head injury have
significantly higher serum glucose levels than those with
Fluid and Electrolytes moderate injury, and those with significantly higher
glucose levels have an unfavorable outcome. Among the
Electrolyte abnormalities are common in patients with
patients with more severe head injury, a glucose level
head injuries and occur at least once during
greater than 200 mg/dl was associated with a worse
hospitalization72. The most common abnormalities seen
outcome. A significant relationship was found between
are hyponatremia, hypernatremia and hypokalemia.
postoperative glucose levels, pupillary reaction and
Hyperglycemia is also common and is frequently seen
maximum intracranial pressure during the first 24 hours,
and is part of the stress response to injury and should be
and postoperative glucose level was an independent
controlled with the use of insulin and should be kept
predictor of outcome76. Patients with a GCS of 8 or less
below 150mg/dl. Meticulous attention should be paid
had significantly higher serum glucose levels than patients
to fluid management and normal balance established.
with GCS of 12 to 15. Patients who subsequently
Hyponatremia syndromes remained in vegetative state or died had significantly
higher glucose levels both on admission and
The differential diagnosis of hyponatremia in head
postoperatively than patients who had good outcome or
injured patients consists of two entities – syndrome of
moderate disability. Severely head-injured patients
inappropriate antidiuretic hormone secretion (SIADH)
frequently develop hyperglycemia and the elevated serum
and cerebral salt wasting syndrome (CSWS). The
glucose levels above 200 mg/dl may aggravate ischemic
diagnosis of SIADH requires the following criteria:
insults and worsen neurological outcome in these patients.
serum sodium less than 135 mEq/L, serum osmolarity
Blood glucose is associated with brain tissue acidosis in
less than 289 mOsm/L, urine osmolarity greater than
severe TBI. Insulin therapy significantly reduced the
serum, specific gravity exceeding 1010 and an
blood glucose levels but the brain tissue pH did not change
inappropriately elevated urinary sodium. In CSWS,
much, though there was a suggestion of improvement if
serum sodium should be less than 135mEq/L, osmolarity
the change in blood glucose was large77.
less than 280 mOsm/L, urinary sodium more than 25
mEq, specific gravity exceeding 1010 .The volume status Intensive insulin therapy titrated to maintain blood
is the critical clinical distinction, there being an increased glucose level between 4.4 and 6.1 mmol/l during intensive
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
Intensive Care Management of the Head Injured Patient 91
care unit stay has been shown to significantly decrease four therapies that target multiple mechanisms of cerebral
mortality, septic morbidity, sepsis-related organ failure, ischemia , neurotoxic cascades , inflammation and brain
transfusion requirements and polyneuropathies. swelling and will play a significant role in the future .
Hyperglycemia on admission is related to susceptibility
REFERENCES
to infections and worse outcomes following myocardial
and cerebral ischemic events. Additional beneficial effects
of insulin, unrelated to the control of glycemia, have 1. Eyester E, Watts C. An update of the National Head and
also been reported and need to elucidated further78. Spinal Cord Injury Prevention Program of the American
Association of Neurological Surgeons and the Congress of
Transient hyperglycemia affected cerebral energy Neurological Surgeons.
metabolism at blood glucose concentration above 15 Clin Neurosurg 1992; 38:252-60.
mmol/l has been shown by a moderate increase in 2. Avolio AEC, Ramsey FL, Neuwelt EA. Evaluation of a program
interstitial lactate level. Moderate hyperglycemia did not to prevent head and spinal cord injuries: a comparison between
change intracerebral levels of lactate, pyruvate, glutamate, middle and high schools.
glycerol, or lactate/pyruvate ratio. Pronounced cerebral Neurosurgery 1992:31:557-562.
lactic acidosis and a moderate increase in interstitial 3. Watson GS, Zador PL, Wilks A. The repeal of helmet use
glycerol concentration indicating cell membrane laws and increased mortality in the United States 1975-1978.
degradation was observed in long-lasting hyperglycemia79. Am J Public Health 1980; 70: 529-85.
4. Thompson RS, Rivara FP, Thompson DC. A case-control
MONITORING study of the effectiveness of bicycle helmets.
Neurological monitoring in the neurointensive care unit N Engl J Med 1989; 320: 1361-7.
is centred around two important secondary injury 5. Kaufman HH, Timberlake G, Voelker J, Pait TG. Medical
processes, elevated intracranial pressure and cerebral complications of head injury.
ischemia. The modalities that are available in a well Med Clin N Amer 1993; 77: 43-60.
established neurocentre are monitoring cerebral 6. Demling R, Riessen R. Pulmonary dysfunction after cerebral
hemodynamics with Transcranial Doppler injury.
Ultrasonography, Laser Doppler Flowmetry and Xenon Crit Care Med 1990; 18: 768-74.
enhanced computed tomography80. Cerebral oxygenation 7. Ott L, McClain CJ, Gillespie M, Young B. Cytokines and
can be monitored by Jugular venous oxygen saturation, metabolic dysfunction after severe head injury.
Near Infrared Spectroscopy and brain tissue oxygen J Neurotrauma 1994; 11: 447-72.
monitoring and neuronal function can be monitored by 8. Goodnight SH, Kenoyer G, Rapaport SI, Patch MJ, Lee JA,
electroencephalography and evoked potentials 81-86. Kurze T. Defibrination after brain tissue destruction.
Intracranial pressure is monitored with an N Engl J Med 1974; 290:1043-7.
intraventricular catheter which will guide therapy. 9. Olson JD, Kaufman HH, Moake J et al. The incidence and
Intracerebral microdialysis is a very useful monitor which significance of hemostatic abnormalities in patients with head
provides information on cerebral metabolism87. injuries.
Neurosurgery 1989; 24:825-32.
CONCLUSION 10. Hulka F, Mullins RJ, Frank EH. Blunt brain injury activates
the coagulation process.
Head injuries are a major cause of morbidity and
Arch Surg 1996; 131:923-8.
mortality especially in the young and is a serious
socioeconomic problem. The aim should be to optimize 11. Stein SC, Young GS, Talucci RC, Greenbaum BH, Ross SE.
Delayed brain injury after head trauma: significance of
the management early so as to enable a favourable
coagulopathy.
outcome. Intensive care treatment should be managed Neurosurgery 1992; 30:160-165.
by monitoring these patients to prevent secondary brain
damage. A well organized secondary brain damage 12. Teasdale GM. Head Injury.
J Neurol Neurosurg Psychiat 1995; 58:526-39.
protocol should be established, with the help of the state
of the art monitoring of cerebral function, so that patients 13. King BS, Gupta R, Narayan RK. The early assessment and
have a favourable outcome. Dexanabinol, hypertonic intensive care unit management of patients with severe
traumatic brain and spinal cord injuries.
saline, decompressive craniectomy and hypothermia are Surg Clin N Amer 2000; 80:855-71.
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
92 V. Bhadri Narayan
14. Fitzpatrick MO, Maxwell WL, Graham DI. The role of the amino acid formula, and nitrogen dose on nitrogen retention
axolemma in the initiation of traumatically induced axonal in traumatic and septic stress.
injury. Ann Surg 1987; 205: 282-7.
J Neurol Neurosurg Psychiat 1998; 64:285-7.
30. Rapp RP, Young B et.al .The favourable effect of early
15. Letarte PB. Neurotrauma care in the new millennium. parenteral feeding on survival in head injured patients .
Surg Clin N Amer 1999; 79:1449-71. J Neurosurg 1983; 58: 906-12.
16. Povlishock JT. Pathobiology of traumatically induced axonal 31. Suchner U, Senftleben U et.al Enteral versus parenteral
injury in animals and man. nutrition :Effects on gastrointestinal function and metabolism.
Ann Emerg Med 1993; 22:980-7. Nutrition 1996; 12: 13-22.
17. Hovda DA, Lee SM, Smith ML, et al. The neurochemical 32. D S Slone. Nutritional support of the critically ill and injured
and metabolic cascade following brain injury: moving from patient.
animal models to man. Crit Care Clin 2004; 20:135-57.
J Neurotrauma 1995; 12:903-6.
33. Brooks MJ, Melnik G. The refeeding syndrome: an approach
18. Gennarelli TA.The pathobiology of traumatic brain injury. to understanding its complications and preventing its
Neuroscientist 1997; 3:73-81. occurrence.
19. Zink BJ. Traumatic brain injury outcome: concepts for Pharmacotherapy 1995; 15:713-26.
emergency care. 34. Weinster RL, Krumdieck CL. Death resulting from
Ann Emerg Med 2001; 37:318-32. overzealous total parenteral nutrition: The refeeding syndrome
20. Marik P, Chen K, Varon J, Fromm R, Sternbach GL. revisited.
Management of increased intracranial pressure: a review for Am J Clin Nutr 1981; 34:393-9.
clinicians. 35. DeGeorgia MA et.al .Prophylaxis of deep vein thrombosis .In
J Emerg Med 1999; 17:711-9. Hacke W et.al (eds): Neurocritical Care.Berlin , Springer-
21. Jaggi JL, Obrist WD, Gennarelli TA, Langfitt TW.Relationship Verlag, 1994; 162-6.
of early cerebral blood flow and metabolism to outcome in 36. Powers SK , Edwards MSB .Prophylaxis of thromboembolism
acute head injury. in the neurosurgical patient : A review.
J Neurosurg 1990;7 2:176-82. Neurosurgery 1982; 10: 509.
22. Marmarou A, Anderson RL, Ward JD, et al. Impact on ICP 37. Shlomi Constantini, Andy Kanner, Adi Freidmen, et al. Safety
instability and hypotension on outcome in patients with severe of perioperative minidose heparin in patients undergoing brain
head trauma. tumor surgery : a prospective randomized double blind study.
J Neurosurg 1991; 75(suppl):S59-S66. J Neurosurg 2001;94: 918-21.
23. Pazzaglia P, Frank G, Frank F, Gaist G. Clinical course and 38. Kamada T, Fusamoto H, Kawano S, Noguchi M, Hiramatsu
prognosis of acute post traumatic coma. K, Masuzawa M, Abe H, Fujii C, Sugimoto T: Gastrointestinal
J Neurol Neurosurg Psychiat 1975; 38:149-54. bleeding following head injury: A clinical study of 433 cases.
24. Gadisseux P, Ward JD : Nutritional support of head injured J Trauma 1977; 17: 44-7.
patients . In Becker DP , Gudeman SK(eds) : Textbook of 39. Peura DA, Johnson LF: Cimetidine for prevention and
Head Injury. Philadelphia , Saunders , 1989; 241-54. treatment of gastroduodenal mucosal lesions in patients in an
25. Van Way CW III. Nutritional support in the injured patient. intensive care unit.
Surg Clin N Amer 1991; 71:537-48. Ann Intern Med 1985; 103:173-7.
26. Wilmore DW. Catabolic illness. Strategies for enhancing 40. Pinilla JC, Oleniuk FH, Reed D, Malik B, Laverty WH:
recovery. Does antacid prophylaxis prevent upper gastrointestinal
N Engl J Med 1991; 325:695-702. bleeding in critically ill patients?
Crit Care Med 1985; 13:646-50.
27. Twayman D. Nutritonal management of the critically ill
neurologic patient. 41. Schuster DP, Rowley H, Feinstein S, McGue MK, Zuckerman
Crit Care Clin 1997; 13:39-49. GR: Prospective evaluation of the risk of upper gastrointestinal
bleeding after admission to a medical intensive care unit.
28. Shaw SN, Elwyn DH, Askenazi J et al. Effects of increasing Am J Med 1984; 76:623-30.
nitrogen intake on nitrogen balance and energy expenditure
in nutritionally depleted adult patients receiving parenteral 42. Shuman RB, Schuster DP, Zuckerman GR: Prophylactic
nutrition. therapy for stress ulcer bleeding: A reappraisal.
Am J Clin Nutr 1983; 37: 930-40. Ann Intern Med 1987; 106:562-7.
29. Cerra F, Hirsch J, Mullen K et al.The effect of stress level, 43. Giuseppe Citerio , Manuela Cormia . Sedation in
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
Intensive Care Management of the Head Injured Patient 93
neurointensive care: advances in understanding and practice . J Neurosurg 1983; 59: 455 – 60.
Curr Opin Crit Care 2003; 9: 120-6.
58. Cruickshank JM, Degaute JP, Kuurne T, et al . Reduction of
44. Peter H Tonner , Norbert Weiler , Andrea Paris et.al . Sedation stress/ catecholamine – induced cardiac necrosis by beta
and analgesia in the ICU. blockade.
Curr Opin Anaesthesiol 2003; 16:113-21. Lancet 1987; ii 585-9.
45. Marik P, Chen K, Varon J, Fromm R, Sternbach GL. 59. Kirland LL , Wilson GL. Extracranial effects of acute brain
Management of increased intracranial pressure: a review for injury.
clinicians. Problems in Critical Care 1991;5: 292-306.
J Emerg Med 1999;17:711-9.
60. Demling R, Reissen R. Pulmonary dysfunction after cerebral
46. Narayan RK, Kishore PRS, Becker DP, et al. Intracranial injury.
pressure: to monitor or not to monitor? Crit Care Med 1990; 18: 768-74.
J Neurosurg 1982;56:650-9.
61. Beckman DL, Bean JW, Baslock DR . Neurogenic influence
47. Eisenberg HM, Frankowski RF, Constant RF et.al High dose on pulmonary compliance.
barbiturates control elevated intracranial pressure in severely J Trauma 1974; 14:111-5.
head injured patients.
62. Amato MB, Barbas CS, Medeiros DM, et al. Effect of
J Neurosurg 1988;69; 15-23.
protective ventilation strategy on mortality in the acute
48. Miller JD. Head injury and brain ischaemia – Implications for respiratory distress syndrome.
therapy. N Engl J Med 1998; 338:347–54.
Br J Anaesth 1985; 57;120-9.
63. Ranieri VM, Suter PM, Tortorella C, et al. Effect of mechanical
49. Chestnut RM, Marshall LF, Klauber MR, et al. The role of ventilation on inflammatory mediators in patients with acute
secondary brain injury in determining outcome from severe respiratory distress syndrome.
head injury. JAMA 1999, 282:54–61.
J Trauma 1993;34:216-22.
64. Ross SE, O’Malley KF, DeLong WG, Born CT, Schwab CW.
50. Fearnside M R, Cook RJ et.al. The Westmead Head Injury Clinical predictors of unstable cervical spine injury in multiply
outcome in severe head injury . A comparative analysis of pre- injured patients.
hospital, clinical and CT variables. Injury 1992; 23:317-9.
Br J Neurosurg 1993; 7 : 267-79.
65. Peter Ford, Jerry Nolan.Cervical spine injury and airway
51. Changaris DG, McGraw CP, Richardson JD, Garretson HD, management.
Arpin EJ, Shields CB. Correlation of cerebral perfusion pressure Curr Opin Anaesthesiol 2002; 15:193-201.
and Glasgow Coma Scale to outcome.
66. Bivins HG, Ford S, Bezmalinovic Z, Price HM, Williams JL.
J Trauma 1987;27:1007-12.
The effect of axial traction during orotracheal intubation of
52. Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion the trauma victim with an unstable cervical spine.
pressure: management protocol and clinical results. Ann Emerg Med 1988; 17:25-9.
J Neurosurg 1995;83:949-62.
67. Majernick TG, Bieniek R, Houston JB, Hughes HG. Cervical
53. Rosner MJ, Coley I. Cerebral perfusion pressure: a spine movement during orotracheal intubation.
hemodynamic mechanism of mannitol and the postmannitol Ann Emerg Med 1986; 15:417-20.
hemogram.
68. Rouby JJ, Laurent P, Gosnach M, et al. Risk factors and
Neurosurgery 1987;21:147-56.
clinical relevance of nosocomial maxillary sinusitis in the
54. Rosner MJ, Daughton S. Cerebral perfusion pressure critically ill.
management in head injury. Am J Resp Crit Care Med 1994; 150:776–83.
J Trauma 1990;30:933-41.
69. Koh WY, Lew TWK, Chin NM, Wong MFM. Tracheostomy
55. Graf CJ, Rossi NP .Catecholamine response to intracranial in neurointensive care setting: Indications and timing.
hypertension. Anaesth Intens Care 1997; 25:365–8.
J Neurosurgery 1978; 49: 862-8.
70. Jones PA, Andrew PJD, Midgley S, et al. Measuring the
56. Kong DL, Prough DS, Whitley DM et.al . Haemorrhage and burden of secondary insults in head injured patients during
intracranial hypertension in combination increase cerebral intensive care.
production of thromboxane A2. J Neurosurg Anesthesiol 1994; 6: 4-14.
Crit Care Med 1991; 19: 532-8.
71. Philippe Eggimann, Didier Pittet. Infection control in the
57. Robertson CS , Clifton GL, Taylor AA, et al. Treatment of ICU.
hypertension associated with head injury. Chest 2001; 120:2059-93.
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
94 V. Bhadri Narayan
72. Piek J, Chestnut RM, Marshall LF, et al. Extra cranial 80. MTV Chan, JMK Lam. New monitors of neurological
complications of severe head injuries. functions. Part-1 and 2.
J Neurosurg 1992; 77: 901-7. Curr Anaes Crit Care 1999; 10: 87-97.
73. Satwant K Tiwana Samra. Neuroendocrinolgy. In Maurice S 81. Schell RM, Cole DJ. Cerebral monitoring: jugular venous
Albin (ed). Textbook of Neuroanaesthesia. McGraw-Hill, 165- oximetry.
70. Anesth Analg 2000; 90: 559-66.
74. Young B, Ott I, Dempsey R, et al. Relationship between 82. Vigué B, Ract C, Benayed M, et al. Early SjvO2 monitoring in
admission hyperglycemia and neurologic outcome of severely patients with brain trauma.
brain injured patients. Intens Care Med 1999; 25: 445-51.
Ann Surg 1989; 210: 466-72.
83. Howard L, Gopinath S, Uzura M, et al. Evaluation of a new
75. Lam AM, Wina HR, Cullen BF, et al. Hyperglycemia and fiberoptic catheter for monitoring of jugular venous oxygen
neurological outcome in patients with head injury. saturation.
J Neurosurg 1991; 75: 545-51. Neurosurgery 1999; 44: 1280-5.
76. Rovlias A, Kotsou S. The influence of hyperglycemia on 84. Owen-Reece H, Smith M, Elwell CE, Goldstone JC. Near
neurological outcome in patients with head injury. infrared spectroscopy.
N Neurosurg 1991; 75:545-51. Br J Anaesth 1999; 82: 418- 26.
77. Zygun David A, Steiner Luzius A, Johnston Andrew, et al. 85. Van Santbrink H, Maas AI, Avezaat CJ. Continuous
Hyperglycemia and brain-tissue pH after traumatic brain monitoring of partial pressure of brain tissue oxygen in patients
injury. with severe head injury.
Neurosurgery 2004; 55:877-84. Neurosurgery 1996; 38: 21-31.
78. Schurr Avital. Tight control of glycemia in critically ill patients. 86. Hoffman WE, Charbel FT, Edelman G. Brain tissue oxygen,
Curr Opinion inClin Nutr Met Care 2002; 5:533-7. carbon dioxide, and pH in neurosurgical patients at risk for
ischemia.
79. Pedro Diaz-Parejo, Nils Ståhl, Wangbin Xu, Peter Reinstrup,
Anesth Analg 1996; 82: 582-6.
Urban Ungerstedt, Carl-Hendrik Nordstrom. Cerebral energy
metabolism during transient hyperglycemia in patients with 87. Valadka A, Goodman JG, Gopinath S, et al. Comparison of
severe brain trauma. brain tissue oxygen tension to microdialysis-based measures
Intens Care Med 2003; 29:544-50. of cerebral ischemia in fatally head-injured patients.
J Neurotrauma 1998; 15: 509-19.
Indian Journal of Neurotrauma (IJNT), Vol. 3, No. 2, 2006
You might also like
- Head TraumaDocument15 pagesHead TraumaDede Yusuf FNo ratings yet
- Traumatic Brain InjuryDocument14 pagesTraumatic Brain InjuryBelle CaharopNo ratings yet
- Introduction to Traumatic Brain InjuryDocument25 pagesIntroduction to Traumatic Brain InjuryRyo JamunNo ratings yet
- Treat Concussion, TBI, and PTSD with Vitamins and AntioxidantsFrom EverandTreat Concussion, TBI, and PTSD with Vitamins and AntioxidantsNo ratings yet
- Kargil Untold StoriesDocument214 pagesKargil Untold StoriesSONALI KUMARINo ratings yet
- Julian's GodsDocument162 pagesJulian's Godsअरविन्द पथिक100% (6)
- Adkins, A W H, Homeric Values and Homeric SocietyDocument15 pagesAdkins, A W H, Homeric Values and Homeric SocietyGraco100% (1)
- The Free Little Book of Tea and CoffeeDocument83 pagesThe Free Little Book of Tea and CoffeeNgopi YukNo ratings yet
- English: Quarter 1 - Module 1Document16 pagesEnglish: Quarter 1 - Module 1Ryze100% (1)
- Factors Affecting Job Satisfaction of EngineersDocument35 pagesFactors Affecting Job Satisfaction of Engineerslingg8850% (2)
- Chesnut 2007Document38 pagesChesnut 2007ALVARO ARIASNo ratings yet
- Moderate and Severe Traumatic Brain Injury Pathophysiology and ManagementDocument11 pagesModerate and Severe Traumatic Brain Injury Pathophysiology and ManagementRonald Joy DatuNo ratings yet
- Prehospital TBI JNSDocument11 pagesPrehospital TBI JNSCamilo Benavides BurbanoNo ratings yet
- Neurogenic Shock - Symptoms, Causes and TreatmentDocument6 pagesNeurogenic Shock - Symptoms, Causes and Treatmentzefri suhendarNo ratings yet
- Treatment Options For Posttraumatic Epilepsy: ReviewDocument7 pagesTreatment Options For Posttraumatic Epilepsy: ReviewOmarJoseCuberosMarcanoNo ratings yet
- Jurnal Radiologi 2Document13 pagesJurnal Radiologi 2Altira PanjaitanNo ratings yet
- Management of Traumatic Brain Injury Some CurrentDocument5 pagesManagement of Traumatic Brain Injury Some CurrentDr. Victor Alonso Hernández HernándezNo ratings yet
- MinervaAnestesiol-12294 ProofinPDF V3 2018-03-16Document10 pagesMinervaAnestesiol-12294 ProofinPDF V3 2018-03-16Marcela Sanchez ParraNo ratings yet
- Spinal Injury CordDocument10 pagesSpinal Injury Cordeleanai limaNo ratings yet
- Aaaaa Traumatic Brain Injury in Dogs and Cats A Systematic ReviewDocument13 pagesAaaaa Traumatic Brain Injury in Dogs and Cats A Systematic ReviewStoian AndreiNo ratings yet
- Traumatic Brain Injury in Dogs and Cats: A Systematic ReviewDocument13 pagesTraumatic Brain Injury in Dogs and Cats: A Systematic ReviewLaura MendezNo ratings yet
- Femur Shaft Fracture Fixation in Head-Injured Patients: When Is The Right Time?Document8 pagesFemur Shaft Fracture Fixation in Head-Injured Patients: When Is The Right Time?Noor Syamsu KomarullohNo ratings yet
- Management of Traumatic Brain Injury: Some Current Evidence and ApplicationsDocument4 pagesManagement of Traumatic Brain Injury: Some Current Evidence and ApplicationsAngela PuspitaNo ratings yet
- Brain Injury and OrthopaedicDocument10 pagesBrain Injury and OrthopaedicRaymond WinNo ratings yet
- Traumatic Brain Injury Initial Resuscitation and TransferDocument4 pagesTraumatic Brain Injury Initial Resuscitation and TransferRielc zemartinNo ratings yet
- Brain TEC 2020Document8 pagesBrain TEC 2020CamiTorresNo ratings yet
- Chronic Traumatic Encephalopathy in Professional American Football Players Where Are We NowDocument9 pagesChronic Traumatic Encephalopathy in Professional American Football Players Where Are We Nowwilliam ortizNo ratings yet
- 33 Spinal Cord InjuryDocument17 pages33 Spinal Cord InjuryMiguel SanJuanNo ratings yet
- Cisternostomy: A Timely Intervention in Moderate To Severe Traumatic Brain Injuries: Rationale, Indications, and ProspectsDocument6 pagesCisternostomy: A Timely Intervention in Moderate To Severe Traumatic Brain Injuries: Rationale, Indications, and ProspectsAtul JainNo ratings yet
- DR Mohamed Al Tamiami:5 Class Lecture 1 OnDocument6 pagesDR Mohamed Al Tamiami:5 Class Lecture 1 OnAmmarNo ratings yet
- Critical Care Management of Adult Traumatic Brain InjuryDocument7 pagesCritical Care Management of Adult Traumatic Brain InjuryRielc zemartinNo ratings yet
- Brain Trauma Edeme HGDocument15 pagesBrain Trauma Edeme HGiulia lupascuNo ratings yet
- Kuo 2017Document18 pagesKuo 2017Nathalia Virgínia CordeiroNo ratings yet
- Traumatic Brain Injury: 2. Prophylactic HypothermiaDocument77 pagesTraumatic Brain Injury: 2. Prophylactic HypothermiaNinaNo ratings yet
- Basic Strategy of Therapy for CNS InjuryDocument4 pagesBasic Strategy of Therapy for CNS InjuryDonny HeykelNo ratings yet
- Assessment, Controversy, and Confounding Factors: Brain DeathDocument23 pagesAssessment, Controversy, and Confounding Factors: Brain DeathdewiNo ratings yet
- 1726 6163 2 PBDocument7 pages1726 6163 2 PBrian00019No ratings yet
- Neuroprotección en TEC, Revisión ActualizadaDocument11 pagesNeuroprotección en TEC, Revisión ActualizadaGustavo Delgado ReyesNo ratings yet
- Management Head Injury in ICUDocument5 pagesManagement Head Injury in ICUIrma KusumaNo ratings yet
- Br.J.Anaesth. 2007 Helmy 32 42Document12 pagesBr.J.Anaesth. 2007 Helmy 32 42ilhaniNo ratings yet
- Manage Severe TBI and Prevent Secondary InjuryDocument17 pagesManage Severe TBI and Prevent Secondary InjuryJorge Luis German BecerraNo ratings yet
- Head Injury For NeurologistDocument10 pagesHead Injury For NeurologistAmsal Darmawan DakhiNo ratings yet
- Head Injury For Neurologists: Richard GreenwoodDocument9 pagesHead Injury For Neurologists: Richard GreenwoodPangalanitaNo ratings yet
- Management of Head TraumaDocument15 pagesManagement of Head TraumaBetrice KotanNo ratings yet
- The Primary, Secondary, and Tertiary Brain InjuryDocument10 pagesThe Primary, Secondary, and Tertiary Brain InjuryEko Prasetyo BaruNo ratings yet
- Medsci 07 00047Document17 pagesMedsci 07 00047Jorge MontenegroNo ratings yet
- Trauma CraneoencefalicoDocument18 pagesTrauma CraneoencefalicoUCIADULTO UPEDNo ratings yet
- Precision Medicine Severe Tbi and Icp MangementDocument36 pagesPrecision Medicine Severe Tbi and Icp MangementNoor MohammedNo ratings yet
- Prevention, Treatment, and Monitoring of Seizures in The Intensive Care UnitDocument17 pagesPrevention, Treatment, and Monitoring of Seizures in The Intensive Care Unitanggi abNo ratings yet
- Ketofol As An Anesthetic Agent in Patients With.8Document7 pagesKetofol As An Anesthetic Agent in Patients With.8jossfragolaNo ratings yet
- Tema 1. - Neurotrauma Aproximación Genral y Estrategias de ResuscitaciónDocument17 pagesTema 1. - Neurotrauma Aproximación Genral y Estrategias de ResuscitaciónaniadNo ratings yet
- Tce ManagementDocument10 pagesTce ManagementAlice MironesNo ratings yet
- Taccone 2015Document30 pagesTaccone 2015anggi abNo ratings yet
- University of Baghdad Alkindy College of Medicine Fifth Stage / GroupDocument13 pagesUniversity of Baghdad Alkindy College of Medicine Fifth Stage / GroupNoor Al Zahraa AliNo ratings yet
- Head TraumaDocument10 pagesHead TraumaVlad ZecaNo ratings yet
- Head Trauma: Key ConsiderationsDocument1 pageHead Trauma: Key ConsiderationsNawaid KhanNo ratings yet
- Imaging of Traumatic Brain Injury - RADIOL CLIN N AM 2015Document21 pagesImaging of Traumatic Brain Injury - RADIOL CLIN N AM 2015Nicole Ferreira PiccoliNo ratings yet
- Head TraumaDocument10 pagesHead TraumaБека ЭзугбаяNo ratings yet
- Secondary Brain Injury: Prevention and Intensive Care ManagementDocument6 pagesSecondary Brain Injury: Prevention and Intensive Care ManagementFirah Triple'sNo ratings yet
- InTech-Intensive Care Management of The Traumatic Brain InjuryDocument43 pagesInTech-Intensive Care Management of The Traumatic Brain InjuryYanti YantiNo ratings yet
- MoD Head Injury GuideDocument18 pagesMoD Head Injury GuideDamar SwpNo ratings yet
- Neurological EmergenciesDocument12 pagesNeurological EmergenciesSiti RahayuNo ratings yet
- Fnins 13 01178Document12 pagesFnins 13 01178Hrishit ShahNo ratings yet
- Review Article: The Harmful Effects of Subarachnoid Hemorrhage On Extracerebral OrgansDocument13 pagesReview Article: The Harmful Effects of Subarachnoid Hemorrhage On Extracerebral OrgansnurulmaulidyahidayatNo ratings yet
- 10.2478 - JCCM 2021 0029Document3 pages10.2478 - JCCM 2021 0029Elizabeth CastilloNo ratings yet
- Jurnal Trauma KepalaDocument7 pagesJurnal Trauma KepalaTommysNo ratings yet
- Ambulance Equipment Guidelines June 2012Document13 pagesAmbulance Equipment Guidelines June 2012rickyGKNo ratings yet
- Ambulance EquipmentDocument1 pageAmbulance EquipmentrickyGKNo ratings yet
- Unlock-Guidelines Management HypertensionDocument25 pagesUnlock-Guidelines Management HypertensionrickyGKNo ratings yet
- CR37 4McKinzeyDocument7 pagesCR37 4McKinzeyrickyGKNo ratings yet
- Animal Models TBIDocument11 pagesAnimal Models TBIrickyGKNo ratings yet
- Learners' Activity Sheets: Homeroom Guidance 7 Quarter 3 - Week 1 My Duties For Myself and For OthersDocument9 pagesLearners' Activity Sheets: Homeroom Guidance 7 Quarter 3 - Week 1 My Duties For Myself and For OthersEdelyn BuhaweNo ratings yet
- Inver Powderpaint SpecirficationsDocument2 pagesInver Powderpaint SpecirficationsArun PadmanabhanNo ratings yet
- Kepler's Law 600 Years Before KeplerDocument7 pagesKepler's Law 600 Years Before KeplerJoe NahhasNo ratings yet
- HVDC PowerDocument70 pagesHVDC PowerHibba HareemNo ratings yet
- Branch ListDocument65 pagesBranch Listannamichelle1001No ratings yet
- Introduction To Alternative Building Construction SystemDocument52 pagesIntroduction To Alternative Building Construction SystemNicole FrancisNo ratings yet
- Jillian's Student Exploration of TranslationsDocument5 pagesJillian's Student Exploration of Translationsjmjm25% (4)
- Hidaat Alem The Medical Rights and Reform Act of 2009 University of Maryland University CollegeDocument12 pagesHidaat Alem The Medical Rights and Reform Act of 2009 University of Maryland University Collegepy007No ratings yet
- Discover books online with Google Book SearchDocument278 pagesDiscover books online with Google Book Searchazizan4545No ratings yet
- Bias in TurnoutDocument2 pagesBias in TurnoutDardo CurtiNo ratings yet
- AReviewof Environmental Impactof Azo Dyes International PublicationDocument18 pagesAReviewof Environmental Impactof Azo Dyes International PublicationPvd CoatingNo ratings yet
- Grinding and Other Abrasive ProcessesDocument8 pagesGrinding and Other Abrasive ProcessesQazi Muhammed FayyazNo ratings yet
- Understanding Learning Theories and Knowledge AcquisitionDocument38 pagesUnderstanding Learning Theories and Knowledge AcquisitionKarl Maloney Erfe100% (1)
- UA-Series EN F2005E-3.0 0302Document25 pagesUA-Series EN F2005E-3.0 0302PrimanedyNo ratings yet
- City Government of San Juan: Business Permits and License OfficeDocument3 pagesCity Government of San Juan: Business Permits and License Officeaihr.campNo ratings yet
- Price and Volume Effects of Devaluation of CurrencyDocument3 pagesPrice and Volume Effects of Devaluation of Currencymutale besaNo ratings yet
- Financial Accounting and ReportingDocument31 pagesFinancial Accounting and ReportingBer SchoolNo ratings yet
- M2M RF - RHNDocument3 pagesM2M RF - RHNNur Nadia Syamira Bt SaaidiNo ratings yet
- Cloud Computing Basics and Service ModelsDocument29 pagesCloud Computing Basics and Service ModelsBhupendra singh TomarNo ratings yet
- The Butterfly Effect movie review and favorite scenesDocument3 pagesThe Butterfly Effect movie review and favorite scenesMax Craiven Rulz LeonNo ratings yet
- Dues & Scholarship Section: NotificationDocument6 pagesDues & Scholarship Section: NotificationMUNEEB WAHEEDNo ratings yet
- Government of Telangana Office of The Director of Public Health and Family WelfareDocument14 pagesGovernment of Telangana Office of The Director of Public Health and Family WelfareSidhu SidhNo ratings yet
- Gcu On Wiki PediaDocument10 pagesGcu On Wiki Pediawajid474No ratings yet
- I apologize, upon further reflection I do not feel comfortable advising how to harm others or violate lawsDocument34 pagesI apologize, upon further reflection I do not feel comfortable advising how to harm others or violate lawsFranciscoJoséGarcíaPeñalvoNo ratings yet