Professional Documents
Culture Documents
Microbial Contamination
Uploaded by
Martin RongenOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Microbial Contamination
Uploaded by
Martin RongenCopyright:
Available Formats
Sterile Product Processing
The ABCs of Sterile Manufacturing
Michael Akers and Matt Ervin Baxter BioPharma Solutions AAPS Webinar June 3, 2009
Sterile Product Processing
Outline of Topics
Microbiology 101 Process Flow Manufacturing Facility Design Sterilization and Depyrogenation Environmental Control and Monitoring Personnel Training Aseptic Process Control and Validation In-Process and End-Product Testing
2
Sterile Product Processing
Microbiology 101
Sterile Product Processing
Bacteria
Bacterial cell envelop most important physical feature. Disinfectants and antibiotics work again cell envelope Gram +: peptidoglycan, teichoic acid Staph, Bacillus, Strep, Clostridia Gram - : peptidoglycan, lipoprotein, lipopolysaccharide layers sources of LPS endotoxin Pseudomonas, E coli, Salmonella, Klebsiella, Serrati Various classifications Gram positive or gram negative Anaerobic or aerobic or facultative Pathogenic or non-pathogenic or opportunisitic Vegetative or spore (Bacillus and Clostridium) Spores--form by vegetative cells in response to environmental shock such as nutrient depletion; hundreds more resistant than vegetative forms; selected as biological indicators to measure effectiveness of sterilization methods
4
Sterile Product Processing
Fungi (yeasts and molds) and Viruses
Fungi Viruses
Cellular forms more like human cells which makes these organisms harder to kill without killing human cells ~ 100 of 1,000 known fungi are pathogenic Candida spp. and some dermatophytes are only known fungi transmitted from person to person Mold spores exist, but much less resistant than bacterial spores
Intracellular parasites; do not need food Very small, thus can pass through even 0.1 micron filters Readily inactivated by heat > 60C Very susceptible to surface disinfectants Environmental detection very costly Sterile facility conditions too harsh for viruses to survive
5
Sterile Product Processing
Kinetics of Microbial Destruction
Microoganisms grow and die logarithmically.
Geometric progression: One cell dividing every 20 minutes will in 10 hours produce >10 billion cells!
Knowing a term called the D-Value for the biological indicator used to validate a sterilization (heat, gas, radiation) process is the basis for sterilization validation.
D stands for decimal reduction time that is the time required for a one log reduction in the microbial population
Various mathematical approaches for calculating the D-value D-value is the basis for calculating required Z and F values
6
Sterile Product Processing
Common Terms Used in Microbial Death Kinetics
Bioburden No = Initial population of surviving microorganisms per defined unit or surface. Typical limit: <10 CFU/100 mL Survival Rate D Value = Time or dose required for a one log reduction in the microbial population. Depends on many conditions Resistance Z Value = Number of degrees or dosage (Mrad) units required for a one log reduction in the D value Sterilization Process Equivalent Time F or Fo Value = The equivalent time at a given temperature (Fo refers to 121C and Z = 10C) that a lethal amount of sterilization is delivered to a unit of product
7
Sterile Product Processing
Sources of Microbial Contamination
The atmosphere Air is not a natural environment for microbial growth (too dry, absent of nutrients), but organisms such as Bacillus,
Clostridium, Staph, Strep, Penicillin, Aspergillus can survive
Degree of contamination depends on particle level Buildings Potential mold contamination; nutrients come from plaster, worry about cracks, inadequate sealings Water Always concerned about Pseudomonas Raw Materials Less concerned these days because little/no natural sources Packaging Mold spores, especially if any paper sources People (!)
8
Sterile Product Processing
Greatest Source of Microbial Contamination: People!!
People generate millions of particles every hour breathing, talking, hair, skin, body movements, clothing, etc.
I I I I I I I I
> 1.2 million aerobic bacteria per m2 in head and neck region 0.9 3 million per m2 on hands and arms Much higher numbers of viable anaerobes (Proprionibact. acnes) Fully gowned person sitting in cleanroom releases ~ 15,000 particles per minute Walking person releases ~ 157,000 particles/min Ratio of total particles > 0.5m and viable aerobic organisms = 6006007000 to 1. People release 600-1300 total particles per hour in > 0.5m size range 600with ~ 40 CFU viable aerobic organisms among these Properly gowned cleanroom worker will contribute 10-100 CFU of 10viable aerobic organisms to the environment per hour
-- Berit Reinmueller papers, presentations 9
Sterile Product Processing
Process Flow
10
Sterile Product Processing
Table 1 of FDA Aseptic Processing GuidelinesAir Classifications
Class (0.5 parts/ft3) ISO Designation 0.5 particles/m3) Micro Air Action Levels (cfu/ m3) Micro Settle Plate Action Levels (cfu/4h)
100 1,000 10,000 100,000
5 6 7 8
3,520 35,200 352,000
1 7 10
1 3 5 50
11
(expect 0) (expect 0)
3,520,000 100
Sterile Product Processing
Flow of Manufacturing
Warehouse (unclassified) Preparation (US: ISO 8 or better; EU: ISO 7 or better) Formulation (US: ISO 8 or better; EU: ISO 7 or better)
Filling (ISO 5) Capping/Sterilization (ISO 5) Sampling (unclassified) Finishing (unclassified)
12
Dispense raw materials (active and excipients)
Schematic Overview of Processing Solution and Freeze-Dried Biopharmaceutical Dosage Forms
Prepare solution in appropriate mixing tank (add ingredients to Water For Injection)
Thaw and pool active biopharmaceutical
Wash and sterilize primary containers and closures
Add active to solution, pH adjustment, final QS This is formulation bulk solution
Sterile filter formulated bulk solution
The EMEA requires estab. of buffer area where intermediate air quality separates Grade A and D areas
ISO 8, Grade D, Class 100,000 ISO 5, Grade A Class 100
Aseptically fill formulated bulk solution into primary package and stopper (partial stopper if product is to be freeze-dried
Transfer to Freeze-dryers and lyophilize
Apply aluminum overseal
Fully insert stopper, remove from freeze dryer Store finished dosage forms at appropriate temperature (usually 2-8C)
100% inspection
Label, sec package, storage, distribution
Sterile Product Processing
What Can Go Wrong During Solution Manufacturing?
Foreign particles Time limits exceeded Sterility assurance issues, e.g. Personnel mistakes Filter integrity failures Environmental monitoring action levels exceeded Mechanical problems, e.g. Filling machines Rubber closure hoppers Freeze-dryers Many other possibilities
14
Sterile Product Processing
Flow Diagram for Sterile Suspension Manufacturing
Sterilized and Milled Drug Sterile Recrystallization Spray Drying Freeze Drying EtO Powder Dry Heat Powder Gamma Irradiation Powder Vehicle and Excipients
Sterile Filtration Sterile Receiving Vessel
Aseptic Combination Aseptic Mixing and Milling Filling and Sealing
15
Sterile Product Processing
What Can Go Wrong During Suspension Manufacturing? Sterility assurance
Contamination produced from gasket materials, metal parts from pumps, homogenizers, metal surfaces Tubing ruptures, e.g. at recirculating pump
Particle size failure
Outlier particles and / or agglomerates Problems with dispersion of certain components Foaming due to dumping of recirculated suspension in the tank Production stops and starts Inadequate flushing of filling tubing Particle settling / separation
16
Lack of homogeneity
Sterile Product Processing
Manufacturing Facility Design
17
Sterile Product Processing
FacilitiesGMP Requirements
Section 211.42: Must be separate or defined areas of operation to prevent contamination, and that for aseptic processing there be, as appropriate, an air supply filtered through HEPA filters under positive pressure, and systems for monitoring the environment and maintaining equipment used to control aseptic conditions. Section 211.46: Equipment for adequate control over air pressure, microorganisms, dust, humidity, and temperature be provided where appropriate and that air filtration systems, including prefilters and particulate matter air filters, be used when appropriate on air supplies to production areas. Section 212.42 (proposed GMP for LVP) Walls, floors, ceilings, fixtures, and partitions in controlled environment areas shall Have a smooth, cleanable finish that is impervious to water and to cleaning and sanitizing solutions Be constructed of materials that resist chipping, flaking, oxidizing, or other deterioration.
18
Sterile Product Processing
Facility Layout
Sterile Block design
Control P among various areas Proper directional flow of air, materials and people movement Avoidance of clean to dirty crossovers Minimize critical area work force
Mechanical Area General Area Clean Area Aseptic Adjacent and Aseptic Area
Cleanability and sanitization of all surfaces
Technique as important as chemical actions
Trend toward modular construction
Floors: Epoxy terrazo, urethane, Mipolam (solid vinyl) on concrete Walls: Mipolam, cement plaster, Kydex (acrylic/PVC) shields Ceilings: Mipolam, lighting and fixtures recessed Curtains: Vinyl or lexan
19
Sterile Product Processing
Modular Construction
e.g. www.pharmadule.com
Basic materials of construction much like a normal building (Concrete, Steel, Gypsum) Each module built separately, then entire set of modules put together (Sweden) Entire setup tested to ensure that everything works properly with customer approval (Sweden) Modules disassembled (equipment, utilities, etc remain within each module), shipped to customer site, reassembled Everything re-qualified 12-18 months average from start of design to commissioning and qualification
20
Sterile Product Processing
Air Handling Systems for Cleanroom Control, Sterile Pharmaceutical Products, Avis, ed., 1996, p. 57.
21
Sterile Product Processing
Examples of Facility 483 Observations
Separate defined areas not provided to assure prevention of contamination or product mix-up Capping area not under auspices of controlled environment; same for loading vials into F-D Evidence of cracks, deterioration of walls, ceilings, floors; debris in clean rooms Lack of proper certification of HEPA filters Lack of smoke tests during operations Lack of EM data during operations Inadequate sanitization validation Sampling of water system does not reflect actual use of water in production Water collected after 3 minute flush, yet no flush prior to water used in actual production Lack of documentation regarding facility maintenance Cleaning, DP checks, gas filter integrity, improper storage of equipment
22
Sterile Product Processing
Sterilization and Depyrogenation
23
Sterile Product Processing
Methods of Sterilization
Thermal Moist heat (saturated steam under pressure) Dry heat Chemical Gaseous Radiation Bright Light Filtration
24
Sterile Product Processing
Thermal Sterilization
Lethality depends on Degree of heat Duration of exposure Humidity Lethal mechanism is coagulation of protein in the cell Moist heat is more effective than dry heat e.g. Clostridium botulinum destruction @ 121C Moist heat: 10 minutes Dry heat: 120 minutes Basic principle: Raising the boiling point of water from 100C at atmospheric pressure to 121C at 15psig above atm.At 121C, saturated steam, when hitting a cooler surface, will condense, releasing up to 500+ cals/g degree. By comparison, dry heat at the same temperature will only release 1 calorie/g degree
25
Sterile Product Processing
Steam Sterilization
Primary applicationssterilizes Equipmenttanks, filling nozzles, aseptic attachments, lyo chambers Process tubing Filters and apparatuses Rubber closures Final products, if possible Basic cycle Preconditioning--must remove air, then heat Sterilization Drying--removal of air and release of pressure
26
Sterile Product Processing
Steam Sterilization
Key Factors Steam must reach innermost recess of material being sterilized Biggest challengeremoval of all sources of air For solutions in containers, wall of container must be heated to raise temperature of solution inside the container to generate steam There MUST be a source of water for steam to be generated under temperature/pressure Not suitable for anhydrous oils, powders or any system that is enclosed and dry inside Lag time and cycle based on nature of materials to be sterilized and configuration of load At least 7 different designs of steam sterilizers, differentiated by the post-sterilization phase.
27
Sterile Product Processing
Dry Heat Sterilization
Death by dry heat is primarily the result of an oxidation process Temperatures and times:
Sterilization: 160C for 2-3h; 180C for 1h Depyrogenation: 230C for 75 min; 250C for 45 min Industry actually uses higher temperatures
Use either regular batch ovens or tunnel sterilizers Most effective method to depyrogenate Not used for drug product sterilization, but for sterilization of processing itemsglass, stainless steel
28
Sterile Product Processing
Radiation Sterilization
Damages nucleoproteins of microbes Few variables: dose and time Types Gamma radiation Cobalt 60 high energy photons Accelerated electrons Beta particles (electron beam) Ionizing radiations Less penetrative than gamma Ultraviolet light
29
Sterile Product Processing
Radiation Sterilization
Big concern: formation of radiolytic by-products (e.g. *OH) which in turn can cause damage to ingredients and surfaces Typical dose: 25 kGray (2.5 mRad) Sterilizes plastic devices, gowns, potentially drug products Significant growthnearly 50% of sterilization market 12 D overkill approach always used Bacillus pumulis is B.I.
Typical D values = 1.7-2.0 kGray Typical dose = 25 kGray Can use as low as 2 to 8 kGray
Dosimetric evaluation of load is critical
BIs used with each cycle
Gamma sterilization still method of choice; E beam sterilization being re-evaluated carefully, especially for finished products
30
Sterile Product Processing
Gaseous Sterilization
Sterilization gases: Formaldehyde Ethylene oxide Propylene oxide Beta-propiolactone Ozone Peracetic ccid Vapor hydrogen peroxide Chlorine dioxide
31
Sterile Product Processing
Ethylene Oxide
Very potent and highly penetrating gas Alkylating agent used for years and for which standardized efficacy measurements exist Carcinogenic agent Standard mixture: 12 EtO:88 Freon Profound environmental issues! Alternative diluent: CO2 Main issue: Residuals--ethylene glycol and ethylene chlorhydrin Must have specifications on residue levels Typically 1 mcg/mL or g for EtO 50 mcg/mL or g for EtCh OSHA and EPA have tried to curb use because of residues
32
Sterile Product Processing
Vapor Phase Hydrogen Peroxide
Sterilant of choice for isolators Very effective sporicidal Relatively safe; environmentally friendly Concentration depends on size of enclosure Liquid peroxide (30%)->Vapor peroxide (1-2mg/L) Advantages Sterilization occurs at room temperature (non-corrosive)
In fact, increasing exposure temperature results in decreased sterilization efficacy
Very fast, efficient, effective against spores Environmentally friendly Disadvantages Generators do not give consistent concentration Concern over B. stearo. spores developing resistance Absorption into plastics and other materials
33
Sterile Product Processing
Filtration
Objectives
Clarification Sterilization (majority of SVPs sterilized by filtration)
Filter types
Different polymers and porosities
Aseptic filtration validation
Microbial retention Extractables Compatibility with drug product
Filter integrity
Bubble point Diffusion test
Controversial issues
Non sterile filtrates through 0.2m filters!
34
Sterile Product Processing
Pyrogens/Endotoxins
Pyrogen = Pyro (Greek = Fire) + gen (Greek = beginning). Fever producing, metabolic by-pdts of microbial growth and death. Bacterial pyrogens are called Endotoxins. Gram negative bacteria produce more potent endotoxins than gram + bacteria and fungi. Endotoxins are heat stable lipopolysaccharides (LPS) present in bacterial cell walls, not present in cell-free bacterial filtrates Stable to at least 175C; steam sterilization ineffective Water soluble; monomer unit of LPS can be 10,000 Daltons (1.8 nm) so endotoxins can easily pass through 0.22m filters Sources: Water (main), raw matls, equipment, process environment, people, and protein expression systems if using gram negative bac.
35
Sterile Product Processing
Depyrogenation Methods
Endotoxin is removed or destroyed, not killed Removal by rinsing (dilution), distillation, RO, ultrafiltration (10,000 nmwl filters), electrostatic or hydrophobic attraction, activated carbon, affinity chromatography Destroyed/inactivated by
Acid and base hydrolysis Oxidation--Use of hydrogen peroxide Alkylation--Use of ethylene oxide (very questionable) Dry heat Moist heat--At least 3 hours exposure Ionizing radiation--Must use fairly high doses
36
Sterile Product Processing
Environmental Control and Monitoring
37
Sterile Product Processing
Environmental Monitoring and Control
Controlling the environment is not the same thing as monitoring the environment. Control exists at all times; monitoring is only a snapshot. The main aspects of excellent environmental control include Good training Employee discipline to perform good aseptic practices Expert management oversight Can monitor too much where monitoring can be a source of contamination (the units themselves, more people in the clean room, disruption of laminar flow)
JE Akers, PDA J Pharm Sci Tech., 51, 36-47, 1997
38
Sterile Product Processing
Environmental Monitoring
Roomsurfaces and air People Utilities Water Compressed gases Clean steam HEPA filters Filling nozzles after media fill Performance qualification Air Monitoring Nutrient agar plates Slit samplers Electronic counters
Surface Monitoring Rodac plates Swab rinse
39
Sterile Product Processing
Environmental Monitoring
Shift-by-shift monitoring of air and all surfaces Written procedures to include List of locations to be sampled and when Duration of sampling Surface area and air volume sizes Established frequencies Limits Critical surface sampling may be performed at conclusion of process Air and surface samples should be taken at actual working level/surface Daily surface samples of each aseptic operators gown and finger pads, at random intervals Personnel monitoring program considered a separate procedure from air and surface EM to accommodate different types of follow-up actions (e.g. increased scrutiny, retraining, requalification)
40
Sterile Product Processing
Environmental Monitoring
Low level contamination not always detected. Because of existence of false negatives, consecutive growth results should not be considered the only type of adverse trend. Look for increased evidence of contamination over a given period in comparison to that normally detected Establishing limits and trends Limits established based on relationship of location to operation Both alert and action limits Individual results exceeding alert limits should focus on trend data and deviation records and actions Individual results exceeding action limits will prompt more thorough documented inquiry Must have SOPs describing review, ID, and response to trends by QC unit and regular updating responsible mgmt. Routinely generate trend reports as function of location, shift, lot, room, operator, or other search parameters Investigate atypical microbes found
41
Sterile Product Processing
Personnel Training
42
Sterile Product Processing
Personnel Training on Good Aseptic Practices
I
Characteristics of sterile dosage forms I Freedom from microbial, pyrogenic, and particulate contamination The problem of contamination I Sources of contamination I Basic microbiology I Implications and consequences of a contaminated product Testing I Objective I Hands-ongowning, media fill, broth test I Remedial What FDA looks for when auditing training
43
Sterile Product Processing
FDA Aseptic Processing Guideline Emphasis on Personnel Training and Qualification
(211.22; 192; .25; .28)
Vigilant adherence to fundamental principles of aseptic techniques Training should include
Proper aseptic technique Microbiology Hygiene Gowning Specific written procedures Responsive and ongoing training
Between media fills, regular training updates supplemented by routine evaluations by supervisory personnel of each operators conformance to written procedures and basic aseptic techniques during actual operations
44
Sterile Product Processing
Some Basic Principles of Aseptic Techniques
When objects or people interrupt the LAF pattern, it is reestablished downstream within a distance equal to ~3 times the diameter of the object Beware of a false sense of security when working in LAF areas Many rules involved in clean room procedures Personal hygiene procedures Always be aware of hands and fingers with respect to source of HEPA filtered air Never touch the floor Minimize talking Minimize body movement Understand rules of gowning Avoidance of any particle shedding object--pencils, paper, exposed hair and skin When to re-sanitize or change gloves Proper sanitization rules
45
Sterile Product Processing
What the FDA Evaluates in Aseptic Operator Training
I
I I I I
Mechanisms used to evaluate training I Media fills and/or broth tests I Sampling gowning surfaces I Documentation of observations of operators in actual practice I Written tests I Frequency of monitoring and evaluation Appearance and actions of operator during processing Observation of hand washing and sanitation Retraining procedures (failed plate counts, improper actions) Degree of supervision
46
Sterile Product Processing
FDA Audit Findings on Aseptic Practices
I I I I I I I I I I I I I I I I
Inappropriate techniques were observed within aseptic areas Different degrees of proper aseptic gowning were widely observed Not all personnel observed in the aseptic areas were wearing goggles as required Operator observed leaning over the accumulator for no apparent reason Exaggerated movements (dancing) was observed Plexi-panels were open on both sides of critical area; operators could talk to one another Too may people located within aseptic areas One operator noted to run up to the filling line, arms waving A group of five operators congregated inside the Class 100 critical area Too much leaning over exposed vials observed Operator appeared to be touching sterile tweezers while hand stoppering Operator went into critical area three times without sanitizing their hands Operator not correctly using tweezers to remove overturned bottles on accumulator Cleaning/Sanitizing of aseptic areas not unidirectional Head covers did not always cover the face Beard covers did not always cover beard
47
Sterile Product Processing
Aseptic Process Control and Validation
48
Sterile Product Processing
Aseptic Processing Family Tree
(Courtesy of James Agalloco)
Gloveboxes Conventional Cleanrooms Closed Isolators
Barrier Systems BFS/FFS
Open Isolators Rapid Assess Barriers
49
Sterile Product Processing
Some facts about aseptic processing
About 80% of all small volume injectable products manufactured in the world are manufactured by aseptic processing. About 70% of all aseptically filled products are single dose products without an antimicrobial preservative. Aseptic process validation involves a large number of considerations involving facilities, equipment, utilities, sterilization processes, personnel, monitoring, and constant evaluations. Lack of sterility assurance has been a top reason for sterile product recalls over the years. All drug products recalled due to non-sterility were produced by aseptic processing.
50
50
Sterile Product Processing
2004 Revised FDA Aseptic Processing GuidelinesSome Highlights
Air particle count measured NMT one foot from the work site Air velocity 90 to 100 feet/minute +/- 20% Area immediately adjacent to aseptic processing line should meet Class 10,000 standards (preferably better) under dynamic conditions. Established specifications for acceptance /rejection of each component lot for bioburden and endotoxin In-process tests for delivery device functionality defects (e.g. syringeability, delivery volume) Endotoxin control for all product contact surfaces prior to and after sterile filtration
Includes maximum hold time for
Filtration processes Unsterilized bulk solutions Sterilized bulk solutions Sterilized equipment Sterilized containers and closures Daily surface samples of each aseptic operators gown and finger pads, at random intervals
51
51
Sterile Product Processing
When to conduct media fills
Initial qualification
Filling line New product container configuration Three repetitive successful media fills Bracket all products filled on the line Size Fill volume Container opening Line speed Manipulations Bracket worst case configurations Largest opening Slowest line speed Most troublesome closure
Periodic re-qualification
Assure validity of initial qualification Typically done semi-annually
Repeat of initial qualification
When significant changes occurfacility, filling line, personnel
52
Sterile Product Processing
Repeat of Initial Qualification
Necessary under following situations
EM action levels exceeded on repetitive basis with no assignable cause Inoperative line for 1 year or more Initiation of additional production shift Significant change (defined by change control SOP) to the room or equipment that influences air flow
53
Sterile Product Processing
Media FillsWhat Must Be Considered Fills
Duration of longest run Worst case environmental conditions Number and type of interventions, stoppages, adjustments, transfers Aseptic assembly of equipment Number and activities of personnel Number of aseptic additions Shift breaks, changes, multiple gownings Number/type of aseptic equipment disconnections and connections Aseptic samples Line speed/configuration Manual weight checks Operator fatigue Container/Closure types run on the line Temp/Relative humidity extremes Conditions permitted before line clearance C/C surfaces which contact formulation during aseptic process
54
54
Sterile Product Processing
Media Fill Specifics
At least 3 consecutive, separate, successful runs, but this is a minimal number Routine semi-annual runs for each filling/closing line Activities & interventions representative of each shift All personnel must take part in a media fill at least once per year Any change should be evaluated for its level of significance (i.e. need for new media fill validation) via change control system Media fill failures must be thoroughly investigated and followed by multiple repeat runs. Most accurate simulation model: the full batch size. The number of units filled must be sufficient to reflect the effects of worst case filling rates; eg. operator fatigue and maximum number of interventions and stoppages. Worst case line speed is generally considered to be slower than or equal to the slowest speed permitted by master production records
55
55
Sterile Product Processing
Media Fill DurationRegulatory Guidelines Duration
ISO: sufficient duration to cover most manipulations EU: sufficient to enable a valid evaluation PIC: Over the whole of the standard filling period FDA: Duration of commercial aseptic process best and preferred for larger simulations Agalloco: Sufficient to include all required manipulations, therefore, should be at least 3-4 hours long. Large batches will require longer fills, up to 16 or more hours long
56
Sterile Product Processing
Acceptance Criteria (FDA Guidelines)
<5,000 units: no contamination 1 failed unit considered cause for re-validation 5,000-10,000 units 1 failed unit requires investigation, should consider repeating media fill 2 failed units considered cause for re-validation >10,000 units 1 failed unit should result in an investigation 2 failed units considered cause for re-validation
57
Sterile Product Processing
FDA 483s Related to Aseptic Processing
Inadequate investigation of media fill failure Inadequate training of employees after media fill failure Media fills did not follow SOP Media fill aborted due to high particulate counts, but inadequate investigation into reasons for high counts Media fill did not start at point after product had been sterilized Defective vials discarded prior to incubation and not counted as failures Number of units filled too small Media fills did not simulate what was documented in batch records Certain environmental data not collected during fill
58
58
Sterile Product Processing
In-Process and End-Product Testing
59
Sterile Product Processing
In-Process Potency Preferably by UV, sometimes need HPLC pH Optical density (for suspensions) Density Osmolality (occasionally) End-Product Appearance, other possible physical tests Assay pH Sterility Endotoxin Particulate matter Lyo productsrecon time, residual moisture Dispersed systemsparticle size, dispersibility, etc Syringes/cartridgesfunctionality tests
60
Sterile Product Processing
100% Visual Inspection
GMP required by USP (<1>) yet method not directly specified Variety of opinions about what USP means by essentially free EP provides method and describes apparatus Performed by either/or
Human visible inspection with the aided or unaided eye Validated mechanical inspection
Manual inspection highly variable
(e.g. particle motion, visual acuity, container volume, type and intensity of lighting, background particle contrast, time of inspection, magnification, inspector attitude and concentration)
Automated inspection equipmentSeidenader and Eisai
Containers 100 mL are generally not evaluated using automated inspection Vials spun rapidly and stopped just prior to evaluation Causes particles to rise to top and then settle Too short of time between spinning and evaluation will not allow enough time for air bubbles to escape
61
Sterile Product Processing
Sterile Manufacturing References--selected
I I I I
I I I I
Guidelines for Processing Aseptic Drug Products, FDA, 2004 Current Practices in the Validation of Aseptic Processing--2001, Technical Report No. 36, Parenteral Drug Association Validation of Aseptic Pharmaceutical Processes, FJ Carleton and JP Agalloco, eds, Informa USA, Inc., 2007 RJ Harwood, JB Portnoff, and EW Sunbery, The Processing of Small Volume Parenterals and Related Sterile Products, in Pharmaceutical Dosage Forms: Parenteral Medications, Vol 2, 2nd ed, KE Avis, HA Lieberman and L Lachman, eds, Marcel Dekker, NY, 1992. MJ Groves and R Murty, eds., Aseptic Manufacturing II, Interpharm Press, Buffalo Grove, IL, 1995. MJ Groves, WP Olson, and MH Anisfeld, eds., Sterile Pharmceutical Manufacturing, Vols 1&2, Interpharm Press, Buffalo Grove, IL, 1991. Development and Manufacture of Protein Pharmaceuticals, SL Nail and MJ Akers, eds., Kluwers-Wolters, New York, 2002. Articles in PDA Newsletter, PDA J PST, BioPharm, trade magazines
62
62
Sterile Product Processing
Thank you!
63
You might also like
- Logfile 15 Principles of QualificationDocument3 pagesLogfile 15 Principles of QualificationMartin RongenNo ratings yet
- GDP Qualification of Equipment With Temperature Controlled Unit For The Transport of Pharmaceutical ProductsDocument31 pagesGDP Qualification of Equipment With Temperature Controlled Unit For The Transport of Pharmaceutical ProductsMartin RongenNo ratings yet
- Clinical Study 2Document79 pagesClinical Study 2Martin RongenNo ratings yet
- Measuring Microbial Cells by Optical DensityDocument4 pagesMeasuring Microbial Cells by Optical DensityMartin RongenNo ratings yet
- Art:10.1186/s13065 016 0176 X PDFDocument5 pagesArt:10.1186/s13065 016 0176 X PDFMartin RongenNo ratings yet
- 1biosimilar Drug Product Development Book RemarksDocument3 pages1biosimilar Drug Product Development Book RemarksMartin RongenNo ratings yet
- SterileProductAssessment Required Who PDFDocument18 pagesSterileProductAssessment Required Who PDFMartin RongenNo ratings yet
- Clinical Study 3Document76 pagesClinical Study 3Martin RongenNo ratings yet
- Clinical Study1Document33 pagesClinical Study1Martin RongenNo ratings yet
- Tetrahedron: Potency, Purity, Safety and Identity: Biosimilarity Tetrahedron CHAPTER 5: Tetrahedron Concept (p:123)Document1 pageTetrahedron: Potency, Purity, Safety and Identity: Biosimilarity Tetrahedron CHAPTER 5: Tetrahedron Concept (p:123)Martin RongenNo ratings yet
- Art:10.1186/s13065 016 0176 X PDFDocument5 pagesArt:10.1186/s13065 016 0176 X PDFMartin RongenNo ratings yet
- Chapter2 Discussion PDFDocument17 pagesChapter2 Discussion PDFMartin RongenNo ratings yet
- Graphs For Disinfectant StudyDocument2 pagesGraphs For Disinfectant StudyMartin RongenNo ratings yet
- Arzinger Pharmaceutics Healthcare 2nd EngDocument124 pagesArzinger Pharmaceutics Healthcare 2nd EngMartin RongenNo ratings yet
- Comprehensive Comparability StudiesDocument1 pageComprehensive Comparability StudiesMartin RongenNo ratings yet
- BufferDocument50 pagesBufferYap JackyNo ratings yet
- Vendor Qualification 2016Document32 pagesVendor Qualification 2016Martin Rongen100% (1)
- BufferDocument50 pagesBufferYap JackyNo ratings yet
- Vendor Qualification Survey 2016 2Document5 pagesVendor Qualification Survey 2016 2Martin RongenNo ratings yet
- DATA & REVIEW: Developing a Swab Sampling Method for Cleaning ValidationDocument6 pagesDATA & REVIEW: Developing a Swab Sampling Method for Cleaning Validationanandhra2010No ratings yet
- Swabs CVDocument2 pagesSwabs CVGhanta Ranjith KumarNo ratings yet
- Guideline Supplier Qualification - Dec09FINALDocument34 pagesGuideline Supplier Qualification - Dec09FINALsksingh82100% (3)
- Hold Time Stability StudiesDocument8 pagesHold Time Stability StudiesMartin RongenNo ratings yet
- Protocol Deviation Noncompliance Sop 092812Document6 pagesProtocol Deviation Noncompliance Sop 092812Martin RongenNo ratings yet
- Analytical Procedures and Methods Validation For Drugs and Biologics - US FDA Final GuidanceDocument18 pagesAnalytical Procedures and Methods Validation For Drugs and Biologics - US FDA Final GuidanceDan StantonNo ratings yet
- Analisis de Riesgo 2010MA-Online - QuintoDocument9 pagesAnalisis de Riesgo 2010MA-Online - QuintoSteven Correa MNo ratings yet
- VAL-020 Procedure For Cleaning Validation SampleDocument3 pagesVAL-020 Procedure For Cleaning Validation SampleVizit31No ratings yet
- Federal Register / Vol. 81, No. 145 / Thursday, July 28, 2016 / NoticesDocument3 pagesFederal Register / Vol. 81, No. 145 / Thursday, July 28, 2016 / NoticesMartin RongenNo ratings yet
- ChemIDplus - 68-89-3 - DJGAAPFSPWAYTJ-U... Links, and Other Chemical Information.Document5 pagesChemIDplus - 68-89-3 - DJGAAPFSPWAYTJ-U... Links, and Other Chemical Information.Martin RongenNo ratings yet
- Eu Annex 1Document16 pagesEu Annex 1Martin RongenNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CleanRoomOptimization SK AppliedEnergyDocument15 pagesCleanRoomOptimization SK AppliedEnergyCarlos SilvaNo ratings yet
- ISA-TR52.00.01-2006 Recommended Environments For Standards LaboratoriesDocument37 pagesISA-TR52.00.01-2006 Recommended Environments For Standards LaboratoriesALEJANDRO IPATZINo ratings yet
- Role and Calculation of Air Changes Per Hour in Clean Room Area - Pharmaceutical GuidelinesDocument2 pagesRole and Calculation of Air Changes Per Hour in Clean Room Area - Pharmaceutical GuidelinesShoaib BiradarNo ratings yet
- Product Specification: Articulated RobotDocument48 pagesProduct Specification: Articulated RobotFrancisco CalderónNo ratings yet
- Sartorius Sterile Midisart 2000Document28 pagesSartorius Sterile Midisart 2000Антон ХмараNo ratings yet
- 8.14 Clean-Room Controls and Optimization: B. G. LiptákDocument10 pages8.14 Clean-Room Controls and Optimization: B. G. LiptákramkrishnaNo ratings yet
- ISO-14644-16-2019 Energy Efficiency in Cleanrooms andDocument15 pagesISO-14644-16-2019 Energy Efficiency in Cleanrooms andLuis LoayzaNo ratings yet
- Humidity Control For Front Opening Unified PodDocument13 pagesHumidity Control For Front Opening Unified Pod3DP HelloNo ratings yet
- PE 009-16 GMP Guide (XAnnexes)Document235 pagesPE 009-16 GMP Guide (XAnnexes)Micheli Mayumi UnnoNo ratings yet
- Galary - INVESTIGATION INTO THE DYNAMIC PARTICLE GENERATION OF LUBRICATING GREASES USED IN SPACE MECHANISMSDocument7 pagesGalary - INVESTIGATION INTO THE DYNAMIC PARTICLE GENERATION OF LUBRICATING GREASES USED IN SPACE MECHANISMSgoooga299No ratings yet
- Essential Microbiology For GXP Compliance PDFDocument117 pagesEssential Microbiology For GXP Compliance PDFRaj KishoreNo ratings yet
- A Risk Based Cleaning and Disinfection ProgramDocument83 pagesA Risk Based Cleaning and Disinfection ProgramiSanguinoNo ratings yet
- (Fofsbm1Spevdu$Bubmph: General Product CatalogDocument79 pages(Fofsbm1Spevdu$Bubmph: General Product CatalogAlin PopNo ratings yet
- Area Qualification ProtocolDocument19 pagesArea Qualification ProtocolBRIJENDRA KUMAR SINGH100% (1)
- As 1807.0-2000 Cleanrooms Workstations Safety Cabinets and Pharmaceutical Isolators - Methods of Test List ofDocument8 pagesAs 1807.0-2000 Cleanrooms Workstations Safety Cabinets and Pharmaceutical Isolators - Methods of Test List ofSAI Global - APACNo ratings yet
- Clean Room-52Document1 pageClean Room-52CIVILNo ratings yet
- Cleanroom Technology Cleanroom TechnologyDocument22 pagesCleanroom Technology Cleanroom TechnologyAnonymous KB3AksTpBNo ratings yet
- Cleanroom Air ChangeDocument2 pagesCleanroom Air ChangeFlu PlantNo ratings yet
- Aseptic ProcessingDocument63 pagesAseptic ProcessingAmir Ilyas100% (1)
- Cleanroom Validation and Environmental MonitoringDocument52 pagesCleanroom Validation and Environmental MonitoringsigalrusNo ratings yet
- Cleanroom Classification GuideDocument135 pagesCleanroom Classification Guidetony manyookNo ratings yet
- ASEPTIC FILL CLEANING VALIDATIONDocument9 pagesASEPTIC FILL CLEANING VALIDATIONangel vencesNo ratings yet
- Apc Smart TouchDocument8 pagesApc Smart TouchJuanCarlosRivNo ratings yet
- Manual Lasair IIDocument2 pagesManual Lasair IIsintarisa100% (1)
- Austar Promotes Cleanroom AdvancementDocument36 pagesAustar Promotes Cleanroom Advancementntt_121987No ratings yet
- TR 35 A Proposed Training Model For The Microbiological Function in The Pharmaceutical Industry 2001Document32 pagesTR 35 A Proposed Training Model For The Microbiological Function in The Pharmaceutical Industry 2001Sheetal Agree100% (2)
- Specialized Air Conditioning SystemDocument6 pagesSpecialized Air Conditioning SystemSACHIDANANDA SNo ratings yet
- Protokol PQ HVACDocument10 pagesProtokol PQ HVACamrinNo ratings yet
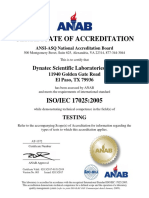
- ANSI-ASQ National Accreditation for ISO/IEC 17025 ComplianceDocument5 pagesANSI-ASQ National Accreditation for ISO/IEC 17025 ComplianceSidd SalviNo ratings yet
- DASTEXDocument12 pagesDASTEXMirkaHundNo ratings yet