Professional Documents
Culture Documents
Chol
Uploaded by
tareetareeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chol
Uploaded by
tareetareeCopyright:
Available Formats
EJCTA - Volume 4 Number 2 December 2010
Cold laser and lipid profile
EFFECT OF LOW-LEVEL LASER THERAPY ON CHOLESTEROL AND TRIGLYCERIDE SERUM LEVELS IN ICU PATIENTS: A CONTROLLED, RANDOMIZED STUDY
Tarek Ali Rushdi, MD
Department Of Anesthesia, Cairo University
Introduction:
igh cholesterol serum levels increases risk of coronary artery disease. To reduce this risk, statins, which is not devoid of side effects in ICU patients, have been prescribed to inhibit the enzyme responsible for cholesterol synthesis. It was proposed that Low-level laser therapy (LLLT) may reduce cholesterol and triglyceride serum levels. This randomized, controlled study investigates the influence of LLLT on the noninvasive reduction of cholesterol and triglyceride serum levels in ICU. Materials and Methods: Twenty ICU patients, 10 in each group, were enrolled in the study. The study group used ilipo LLLT device with 4 laser pads strapped around patient abdomen emitting 650 -660 nm (red) laser light. The control group received sham laser. The laser therapy sessions were done for 55 minutes, twice weekly for two successive weeks with 3 days between sessions. Blood samples were drawn prior to the laser administration. A standard lipid panel was studied before the procedure to establish a baseline and at the end of the second procedure week. The serum triglyceride and total cholesterol and low and high density lipoproteins levels before and after the LLLT were compared. Results: The total cholesterol and serum triglycerides levels in the study group revealed a statistically significant mean change of 15.43 and 13.7 respectively between study baseline and endpoint (P <0.05). Conclusion: The potential application of the noninvasive chemical-free LLLT for cholesterol and triglyceride reduction tended to show favorable results in ICU patients Keywords: Laser, low level; cholesterol, lipoproteins; triglycerides
EJCTA - Volume 4 Number 2 December 2010
Cold laser and lipid profile
Introduction: An obvious relationship exists between increased serum cholesterol levels and coronary heart disease events and the mortality rates attributed to it.1 Moreover, elevated cholesterol levels have been associated with different co-morbidities including stroke, atherosclerosis and myocardial infarction.1 Mostly all of the cholesterol within our bodies arises via biosynthesis. Therefore, physicians aim to reduce cholesterol level in blood by prescribing statins, to decrease the liver and tissue synthesis of cholesterol with resultant decrease in its bioavailability for the synthesis of very low-density lipoproteins which ultimately become low-density lipoproteins. 2-7 Effectiveness of statins in lowering cholesterol concentrations and reducing coronary heart disease risks as well other co-morbidities associated with hypercholesterolemia was revealed in many studies.7-10 However, side effects have been attributed to statins with The American Heart Association unveiling several types of muscle disorders associated with statins: myalgia, mysoitis, and rhabdomyolysis with concomitant creatine kinase elevation and these were proved in several studies.11 It has been revealed that Low-level laser therapy (LLLT) alters gene expression, 12 involved in the biosynthetic cholesterologenesis process. This randomized, controlled study was performed to assess the effectiveness of low level laser therapy in the reduction of cholesterol and triglyceride serum levels non-invasively and without any chemicals or medications. Material and Methods: Twenty ICU patients, divided into two equal groups, were enrolled in this study. The study protocol was approved by the local hospital ethical committee. Written consents were taken from all patients or their next of kin whenever applicable. Randomization was done using a computer generated randomization block. The study members taking the patient samples and performing the analysis were blinded to the patient group allocation. Studied patients were 18 - 75 years old. Patients main diagnostics included cerebrovascular stroke, aortic aneurysm, and fracture base of skull as well as chronic obstructive
2
airway disease. Patients were excluded if body mass index of 30 kg/m2 or greater; have any wound or external trauma to the areas to be treated with the laser; pregnant, breast-feeding, was receiving or received any cholesterol or triglycerides lowering therapy within the last 2months before the study, if were administered any lipid formulation or propofol or if ICU stay was less than 2 weeks. Study group (n=10) received cold low level laser treatment while control group (n=10) received sham laser. The device used was ilipo low level laser machine (Chromogenex, South Wales, United Kingdom) (Figure 1) emitting laser wavelength 650660nm (red laser light) and delivering total energy output of 1.3 W through 38 laser diodes. Four laser pads were securely strapped around the patient abdomen at level of the umbilicus with patient in recumbent position for 55 minutes twice a week for two weeks with three days in between sessions. Patient abdomen was covered with a blanket before laser is on to avoid patient and ICU personnel eye exposure to laser beam. Sham laser was performed using the same device but after covering its pads skin sensors with white plasters rendering laser pads non-functioning as these would not activate laser triggering except when in direct contact with patient skin.
Figure 1: The ilipo Low Level Laser Device
Study Design: Blood samples were drawn prior to the laser treatment phase to obtain a standard lipid profile at baseline. Lipid profiles were attained at 2 different time intervals: pre-procedure and at the end of the second week. The laser administration phase of the study began immediately following the pre-procedure blood sample drawn. The study
EJCTA - Volume 4 Number 2 December 2010
Cold laser and lipid profile
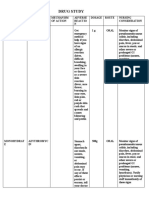
protocol lasted 2 successive weeks, with each patient receiving 4 total procedure administrations with the laser pads throughout 2 weeks (2 procedures per week, each one 3 days apart). The ilipo laser device was activated for 55 minutes each session. The purpose of this randomized, controlled study was to investigate the influence of low level cold laser on serum triglyceride, total cholesterol and low density and high density lipoproteins levels in ICU patients after completion of the 2-week protocol. A power analysis indicated that a minimum sample size of 20 patients randomly assigned to the treatment groups would provide 80% power for detecting a significant difference between the groups. The sample size calculations were performed using the nQuery Advisor software package (version 4.0; Statistical Solutions, Boston, MA). Statistical Analysis: Table 1: Demographic data
Group Study (n = 10) Age(years) mean(SD) Range 47(15) 23-65 25-71 Sex M 5 6 F 5 4 Weight(Kg) mean(SD) 71(12) 68(18)
Results were expressed as means +/- SD. Daily comparisons between study and control groups as regards parametric data were analyzed using unpaired Student t-test. For all statistical comparisons, a P value of <0.05 was considered significant. All statistical analysis was performed using Excel and SPSS 16 package. Results: There was no statistical difference between groups with respect to anthropometric and demographic data (Table 1). There were 6 ventilated patients in the study group versus 4 patients who needed ventilation at any time throughout the ICU stay in the control group with no statistical significance between groups as well. No significant changes were either revealed between studied groups as concerns lipid profile at baseline of the study.
Height(cm) APACHE II Range mean(SD) Range mean(SD) Range 56-107 168(6) 150- 179 18(2) 16-22 60-104 164(7) 160-182 18(2) 17-22
Control (n = 10) 52(14)
80% of the patients who demonstrated an overall reduction in total cholesterol serum levels when comparing pre-procedure and post-procedure Levels were in the study group, though care must be considered due to the small sample size. Table 2 reveals total cholesterol levels at baseline and at the end of the study.
Table 2: Mean and Standard Deviation of Total Cholesterol at Baseline and at the End of Study Group Preprocedure Total Cholesterol Level (mg/dL) Mean SD 198.22 35.34 195.34 22.13 Postprocedure Total Cholesterol Level (mg/dL) Mean SD 182.79 32.35 193.55 42.25 Change in Total Cholesterol Levels (mg/dL) Mean range -15.43 2.0 to -31.0 -1.79 +3.0 to -10 P value
Study (n = 10) Control (n = 10)
< 0.01 >0.05
Low density lipoproteins measurements, on comparing its mean change from baseline to study endpoint in the study group, revealed a reduction of 8.15 points, (P < 0.05; Table 3).
EJCTA - Volume 4 Number 2 December 2010
Cold laser and lipid profile
Table 3: Mean and Standard Deviation of Low Density Lipoprotein (LDL) at Baseline and at the End of Study Group Preprocedure LDL Level (mg/dL) Mean SD 105.68 35.41 123.21 33.21 Postprocedure LDL Level (mg/dL) Mean SD 97.53 28.54 121.30 22.55 Change in LDL Levels (mg/dL) Mean Range 8.15 1.0 to 30.0 -1.91 +1.0 to -12 P value
Study (n = 10) Control (n = 10)
<0.05 >0.05
70% of the patients who demonstrated an overall reduction in low density lipoprotein levels when comparing pre-procedure and post-procedure levels were in the study group. The high density lipoproteins levels in the study group revealed a statistically insignificant mean change of 0.92 between study baseline and endpoint (P > 0.05; Table 4). 75% of the patients who demonstratedan overall reduction in high density lipoprotein levels when comparing pre -procedure and post-procedure levels were in the control group.
Table 4: Mean and Standard Deviation of High Density Lipoprotein (HDL) at Baseline and at the End of Study Group Preprocedure HDL Level (mg/dL) Mean 67.13 64.43 Postprocedure HDL Level (mg/dL) Mean SD 66.21 13.43 60.55 12.45 Change in HDL Levels (mg/dL) Mean Range 0.92 +0.1 to 3.0 -3.88 -2.0 to -8.0 P value
Study (n = 10) Control (n = 10)
SD 14.12 17.21
> 0.05 < 0.05
In the study group patients, a favorable improvement was obvious when comparing the baseline ratio of LDL to HDL levels with the study endpoint ratio, with LDL levels decreasing by 8.15 points and HDL numbers reducing by just 0.92 points; however, the improvement in the LDL to HDL ratio did not reach statistical significance (P > 0.05). The serum triglyceride levels in the study group revealed a statistically significant mean change of 13.7 between study baseline and endpoint (P <0.05; Table 5). 85% of the patients who demonstrated an overall reduction in serum triglyceride levels when comparing pre-procedure and post-procedure levels were in the study group.
Table 5: Mean and Standard Deviation of Serum Triglyceride Level at Baseline and at the End of Study Group Preprocedure Serum Triglyceride Level (mg/dL) Mean SD 83.39 25.97 Postprocedure Serum Triglyceride Level (mg/dL) Mean SD 69.69 26.88 Change in Serum Triglyceride Levels (mg/dL) Mean Range 13.7 3.0 to -21.0 P value
Study (n = 10)
< 0.05
EJCTA - Volume 4 Number 2 December 2010
Cold laser and lipid profile
Control (n = 10)
88.52
23.23
87.33
25.34
-1.19
+1.0 to -13.0
> 0.05
In the study group, none of the patients demonstrated an unsafe increase in triglyceride levels exceeding 150 mg/dL. enhancing further studies to accurately elaborate its therapeutic applicability and utility. Discussion: This randomized, controlled study revealed that LLLT 2 times per week for 2 weeks can reduce cholesterol and triglyceride levels and more References: importantly, reduce LDL levels while preserving HDL levels.
1.
Studies demonstrated that following low level laser irradiation, the mitochondrial membrane potential and proton gradient increases, resulting in mitochondrial optical properties changes with resultant increase in ADP-ATP exchange rate .13 It is also postulated that low level laser therapy increases the electron transfer rate from cytochrome C to dioxygen by cytochrome C oxidase. 14, 15 Subsequently, a gradual shift toward a more oxidized state has been proved; more importantly, the activation of redox-sensitive transcription factors with ultimate gene expression.16, 17, 18 It has been noted that terminal enzymes photoactivation may be the primary response inducing cholesterologenesis suppression. It has also been shown that the initial physical and/or chemical changes of cytochrolme C oxidase alter the intracellular redox state. 19 The latter is proposed to regulate cellular signaling pathways which control gene expression.16.20 Significant reduction in cholesterol and triglyceride levels following the administration of laser therapy with identifiable parameters regarding wavelength, intensity, and frequency was revealed in this study. Even though a statistically significant majority revealed a total cholesterol and triglyceride levels reduction, some patients did not reveal a reduction. This could be attributed to the procedure itself, variability in cholesterol levels, or perhaps mandating crucial alteration in patients dietary habits. Finally, this study provides a fruitful perspective concerning the potential application of this therapeutic noninvasive, chemical-free and medicine-free modality in ICU patients and
5
2.
3.
4.
5.
6.
7.
8.
American Heart Association, Cholesterol Abnormalities & Diabetes, Available at: www.americanheart.org, Accessed September, 2010. Haffner SM, Alexander CM, Cook TJ, et al. reduced coronary events in simvastatin-treated patients with coronary heart disease and diabetes or impaired fasting glucose levels: subgroup analyses in the Scandinavian Simvastatin Survival Study. Arch Intern Med. 1999; 159:2661-2667. Pyorala K, Pedersen TR, Kjekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care. 1997; 20:614-620 Grundy SM. Statin trials and goals of cholesterollowering therapy. Circulation. 1998; 97: 14361439. Rubins HB, Robins SJ, Collins D, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs HighDensity Lipoprotein Cholesterol Intervention Trial Study Group. N Engl J Med.1999; 341:410-418. Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipidlowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004; 291: 1071-1080. Sever PS, Dahlf B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lowerthan average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial. Lipid Lowering Arm (ASCOT-LLA): a multicentre randomized controlled trial. Lancet. 2003; 361:1149-1158. Shepherd J, Cobbe SM, Ford I, et al. West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995; 333:1301-1307.
EJCTA - Volume 4 Number 2 December 2010
Cold laser and lipid profile
9.
10.
11. 12.
13.
14.
15.
16.
17.
18.
19.
20.
Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002; 360: 1623-1630. Stamler J, Daviglus ML, Garside DB, et al. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA. 2000; 284(3):311-318. Thompson PD, Clarkson P, Karas RHJAMA. Statinassociated myopathy. 2003; 289(13):1681-90. Byrnes KR, Wu X, Waynant RW, Ilev IK, Anders JJ. Low power laser irradiation alters gene expression of olfactory ensheathing cells in vitro. Lasers Surg Med. 2005;37: 161-171 Alexandratou E, Yova D, Handris P, Kletsas D, Loukas S. Human broblast alterations induced by low power laser irradiation at the single cell level using confocal microscopy. Photochem Photobiol Sci. 2002; 1:547-552. Hashmi JT, Huang YY, Sharma SK, Kurup DB, De Taboada L, Carroll JD, Hamblin MR, Effect of pulsing in low-level light therapy. Lasers Surg Med. 2010; 42(6):450-66. Huang YY, Chen AC, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy, Dose Response, 2009; 7(4):358-83. Bertoloni G, Sacchetto R, Baro E, Ceccherelli F, Jori G. Biochemical and morphological changes in Escherichia coli irradiated by coherent and noncoherent 632.8 nm light. J Photochem Photobiol. 1993; 18: 191-196. Calkhoven CF, Ab G. Multiple steps in the regulation of transcription factor level and activity. Biochem J. 1996; 317: 329-342. Zhang Q, Piston DW, Goodman RH, Regulation of corepressor function by nuclear NADH. Science. 2002; 295:1895-1897 Tiina Karu. Mechanisms of Low-Power Laser Light Action on Cellular Level Lasers in Medicine and Dentistry. Ed. by Z.Simunovic, Vitgraf: Rijeka, 2000, pp. 97-125 Brown GC. Control of respiration and ATP synthesis in mammalian mitochondria and cells. Biochem J. 1992; 284: 1-13.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2322 Part B DCHB IndoreDocument278 pages2322 Part B DCHB Indoreksanjay209No ratings yet
- Review Article On History of LM Potency - Tracing Its Roots in The PastDocument6 pagesReview Article On History of LM Potency - Tracing Its Roots in The PastRenu BalaNo ratings yet
- How Brain Science Can Inform Architectural DesignDocument12 pagesHow Brain Science Can Inform Architectural DesignadrianmoleavinNo ratings yet
- Effectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuDocument6 pagesEffectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuRizwan KhanNo ratings yet
- Analytical Standardization of Brahmi Nei and Effect of Siddha Methodologies On Spasticity in Cerebral PalsyDocument8 pagesAnalytical Standardization of Brahmi Nei and Effect of Siddha Methodologies On Spasticity in Cerebral PalsytrinitysugumarNo ratings yet
- Drug Study HazDocument7 pagesDrug Study HazRichard HazNo ratings yet
- Managing The Myths of Health Care PDFDocument5 pagesManaging The Myths of Health Care PDFkaremNo ratings yet
- Public Notice Dated 16.11.2018-Disability-AppendixHDocument4 pagesPublic Notice Dated 16.11.2018-Disability-AppendixHDisability Rights AllianceNo ratings yet
- Attachments For Overdentures PDFDocument88 pagesAttachments For Overdentures PDFHugoMoralesTecnicoDental100% (1)
- Medication Errors After Hospital DischargeDocument2 pagesMedication Errors After Hospital Dischargebangbambang wahyudiNo ratings yet
- The Behavioral Medicine Treatment Planner - Douglas E. DeGood & Angela L. Crawford & Arthur E. JongsmaDocument283 pagesThe Behavioral Medicine Treatment Planner - Douglas E. DeGood & Angela L. Crawford & Arthur E. JongsmaSergio Mora88% (8)
- Informed Consent TimetableDocument11 pagesInformed Consent TimetableAkita C.No ratings yet
- Managing dental patients with cardiovascular diseasesDocument54 pagesManaging dental patients with cardiovascular diseasesSafiraMaulidaNo ratings yet
- Pharmacy Math CalculationsDocument8 pagesPharmacy Math CalculationsRahmawati KuswandiNo ratings yet
- Understanding the Immunogenic Properties of VirusesDocument41 pagesUnderstanding the Immunogenic Properties of VirusesMaruf Raza DarubagiNo ratings yet
- Aspirin: The widely used pain reliever and fever reducerDocument4 pagesAspirin: The widely used pain reliever and fever reducerEithel EithelNo ratings yet
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocument8 pagesThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNo ratings yet
- Bench MarkingDocument16 pagesBench MarkingNorj BaraniNo ratings yet
- Acute Myocardial InfarctionDocument35 pagesAcute Myocardial Infarctionvirnzrobz80% (10)
- 9700 w14 QP 23Document16 pages9700 w14 QP 23rashmi_harryNo ratings yet
- Infographic ProteinDocument1 pageInfographic ProteinMichele MarengoNo ratings yet
- Ubd Stage 1-3Document24 pagesUbd Stage 1-3api-336167164No ratings yet
- UrinalysisDocument16 pagesUrinalysisJestha Parayno De Vera100% (6)
- Cold TherapyDocument27 pagesCold Therapybpt2100% (1)
- Obstetric Emergencies: Review Questions: Self-Assessment in Emergency MedicineDocument3 pagesObstetric Emergencies: Review Questions: Self-Assessment in Emergency MedicineMelissa Aina Mohd YusofNo ratings yet
- Low Fat Diet PlanDocument2 pagesLow Fat Diet Planmelissa_glancNo ratings yet
- Who Unicri Cocaine Project Study 1995Document75 pagesWho Unicri Cocaine Project Study 1995speedheartNo ratings yet
- 3 Radiographic Dental Assessment For The Child Patient PDFDocument21 pages3 Radiographic Dental Assessment For The Child Patient PDFFamodimu Funbi SamuelNo ratings yet
- The Chapeter That Is TissueDocument36 pagesThe Chapeter That Is TissuereemNo ratings yet
- Wound Management ProcedureDocument51 pagesWound Management ProcedureSisca Dwi AgustinaNo ratings yet