Professional Documents
Culture Documents
Or RRL
Uploaded by
Alponce Edal AdagOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Or RRL
Uploaded by
Alponce Edal AdagCopyright:
Available Formats
December 1, 2007 | American Society of Registered Nurses
Teaching Nurses to Stand Up to Surgeons in the OR
The Operating Room Nurses The Operating Room nurses have worked alongside surgeons in the operating room (OR) throughout the history of Medical Science. The role of operating room nurses has evolved from performance of mere vocational functions like sterilization of instruments to that of professional functions (Judith Brumm, 2004). Today, the Operating Room nurse enjoys professional autonomy making reasonably independent and self-governing decisions in practice dealing specifically with the human response to life threatening conditions. Any lack of coordination between the nurses and the surgeons in a theatre results in poor patient care with serious consequences. Thus, it is important to teach nurses to stand up to surgeons in the operating room. This process includes teaching supply chain management, communication, error prevention, aseptic techniques and core concepts. Teaching Supply Chain Management The operating room nurse team usually consists of a scrub nurse who handles all the required instruments for the operation, a circulating nurse to help and trainee nurses apart from highly trained specialty nurses. Supply chain is the lifeline of nurse care in operating rooms. Poor management of supply chain always leads to complications in patients, wasteful expenditure of energy in terms of repeat procedures and time, which is a vital factor in theatres. This also causes delays in interventions, cancellation of surgeries and other lapses. It should be noted that much time is usually lost waiting for the sterilized instruments, cotton and other petty consumables at the table rather than waiting for an oxygen cylinder or ECG monitor. This is especially true when several
health care organizations have adapted the one surgeon working on multiple tables with the support staff taking all other responsibilities like administration of anesthesia and oxygen. Teaching Communication Communication in the operating room among the health care team often pertains to discussions about patient cancellations, sending for the next patient, preparation of the theatre resources, equipments, responsibilities, safety, sterility temperature regulation, and recording data. Although fundamental communication skills have been identified for effective practice in the operating theatre, there are significant barriers to their use because of confusion over clarity of roles and the implications for teamwork (Nestel and Kidd, 2006). Thus, there is a need for educating nurses in the areas of verbal and nonverbal communication, on active listening and the effective use of these communication skills with due attention to the environment in which the communication is taking place. Studies have shown that ineffective team communication causes frequent medical errors in the operating room. A recent study to describe the characteristics of communication failures in the operating room and to classify their effects has elucidated that communication failures in the operating room is composed of a common set of problems that occur in team exchanges pertaining to the content, audience, purpose, and occasion of a communication exchange (Lingard et.al,2004). Teaching Error Prevention Nursing profession is legally and morally accountable. Hence, teaching error prevention is vital. A study to describe the potential sources of errors and error prevention in operating room nurse team by qualitative content analysis has shown that there is a need for teamwork practice, shared responsibility in teams and organized teamwork among operating room nurses (Lipponen et.al, 2005). The study has identified fear of errors, turnover in teams, overtime work and emotional distress as potential factors leading to errors in operating room team. The study has also highlighted how shared responsibility among the familiar teams, safety control and formal documentation of
errors prevent medical errors. The study stresses on the need to educate operating room nurses that will help them learn from errors and teach them more effective ways of reporting incidents. (Lipponen et.al, 2005). Teaching Aseptic Techniques The spread of infection via hands is well established (Larson, 1955). Hand washing is one of the most important procedures for preventing the spread of infection and disease. Hand hygiene is an infection control practice with a clearly demonstrated efficacy and remains the cornerstone of efforts to reduce the spread of infections. Hands play a significant role in breaking the chain of infection, the transmission of infection between patients. Factors that influence hand hygiene compliance include workload and staff shortage, poor facilities and lack of understanding (Taylor, 1978). Therefore, every individual involved in surgical procedures should receive appropriate training in surgical hand hygiene. A recent study (Shelly et.al, 2001) has shown that strains of Pseudomonas aeruginosa isolated from 16 post surgical patients in a health care center were from a single nurse who had an infected thumbnail. A study to define the risk factors of blood contamination and injury to operating room nurses has shown at least fifty percent of the operations resulted in an adverse event where at least one person was contaminated with patient blood (Quebbeman et.al, 1991). Teaching core concepts The operating room nurse has to be taught core concepts to effectively manage emotionally stressful situations. Factors such as strained relationships within surgical teams, concerns about the dignity of the patient and the well-being of the family, exposure to death, trauma and procedures like surgical removal of organs for transplantation add up to emotional distress (Cheryl Regehr, 2004). Recommendations A recent study on the need for advanced training for the operating room team (Aggarwal et.al, 2004) strategies has shown that a simulated operating theatre similar
to the simulated laboratory used in aviation industry will enable assessment and improvement of technical and non-technical performance of the staff in the operating room. The study recommends an assessment by experts situated in a control room adjacent to the simulated theatre where the effect of distractions, equipments and patient crisis situations is defined towards reducing the number of adverse events arising in the real operating room. Riley and Manias (2003) have shown that photography can be used as a means of data generation in clinical nursing settings by taking 'snap-shots' of operating room events. Analysis of these snap shots reveals the outcomes in the operating room and paves way for remedial measures. Douglas et.al (2000), have elucidated the use of video recoding as a means to monitor the surgical procedures and team performance to improve outcomes. To improve the nurse output and the quality of patient care, it is also recommended to make a Time Activity Analysis. A Time Activity Analysis helps to lists out all the daily activities and the time spent on them in a theatre (Baylis et.al, 2006). Conclusion Any adverse medical event in an operating room can lead nurses to serious legal consequences and affect their professional future. Hence, it is absolutely important to teach operating room nurses to stand up to surgeons on all the vital aspects discussed. Further, it is also essential to educate nurses to adapt an evidence based approach with the ingredients of critical thinking and emotional intelligence in their practice. References Aggarwal, S Undre, K Moorthy, C Vincent, A Darzi. (2004). The simulated operating theatre: comprehensive training for surgical teams. Qual Saf Health Care; 13:27-32. Baylis, Wendy E Adams, David Allenand, Scott G Fraser. (2006). Do Variations in the Theatre Team Have an Impact on the Incidence of Complications? BMC Ophthalmology 6:13.
You might also like
- Legal Aspects of Nursing - An Important Necessity for NursesDocument4 pagesLegal Aspects of Nursing - An Important Necessity for Nursesgladz25No ratings yet
- NCP HomeworkDocument6 pagesNCP HomeworkAndrea Albester GarinoNo ratings yet
- Intramuscular Injection TechniquesDocument6 pagesIntramuscular Injection TechniquesreinNo ratings yet
- Written Report:: Transitional Human ShelterDocument7 pagesWritten Report:: Transitional Human ShelterKasandra Dawn Moquia BerisoNo ratings yet
- Leptospirosis: Causes, Incidence, and Risk FactorsDocument6 pagesLeptospirosis: Causes, Incidence, and Risk FactorsJackii DoronilaNo ratings yet
- NCP OsteosarcomaDocument6 pagesNCP OsteosarcomaNiksNo ratings yet
- Spontaneous Abortion Final PaperDocument11 pagesSpontaneous Abortion Final Paperapi-241242357No ratings yet
- Reaction Paper ERDocument1 pageReaction Paper ERVann Anthony FuentesNo ratings yet
- Patient ChartDocument2 pagesPatient ChartHydieNo ratings yet
- Chest Injury QuestionsDocument3 pagesChest Injury QuestionsNicole Genevie MallariNo ratings yet
- TAHBSO Procedure OverviewDocument4 pagesTAHBSO Procedure OverviewAlianna Kristine OhNo ratings yet
- HPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDocument21 pagesHPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDaffa IbnurasyNo ratings yet
- Patient SafetyDocument16 pagesPatient Safetyviola septina50% (2)
- Thyroid Papillary Carcinoma CaseDocument6 pagesThyroid Papillary Carcinoma CaseRandy F BabaoNo ratings yet
- Chapter 3 Client PresentationDocument4 pagesChapter 3 Client PresentationEllePeiNo ratings yet
- Villarin Alessandro N40 TMA1Document15 pagesVillarin Alessandro N40 TMA1Zhiela Esteban AbivaNo ratings yet
- Music Art Therapy 2Document9 pagesMusic Art Therapy 2Sharina PaorNo ratings yet
- Core CompetencyDocument9 pagesCore CompetencyCharm BarinosNo ratings yet
- Ethics Case StudyDocument4 pagesEthics Case StudycasscactusNo ratings yet
- Care of Patients With Casts and TractionDocument4 pagesCare of Patients With Casts and TractionRyan Marinay DejarmeNo ratings yet
- Appendectomy InstrumentsDocument47 pagesAppendectomy InstrumentsmoqtadirNo ratings yet
- Group 4 Case PresentationDocument12 pagesGroup 4 Case PresentationAphrill Pearl PacisNo ratings yet
- Nursing Management of Patient with Ovarian CancerDocument7 pagesNursing Management of Patient with Ovarian CancerTerrena Lyn BlackmanNo ratings yet
- Post-op-Case-Conference-DM FootDocument44 pagesPost-op-Case-Conference-DM FootShereen DS Lucman100% (1)
- Vital SignsDocument131 pagesVital SignskasingaNo ratings yet
- A Surgical Case Study On Laparoscopic Cholecystectomy: Page 1 of 29Document29 pagesA Surgical Case Study On Laparoscopic Cholecystectomy: Page 1 of 29Clyde R.OrtegaNo ratings yet
- Worksheet On Moral Deliberation - FinalbDocument4 pagesWorksheet On Moral Deliberation - FinalbEmmanuel ApuliNo ratings yet
- Guide To Making NCPDocument7 pagesGuide To Making NCPKryza Dale Bunado BaticanNo ratings yet
- Final ResearchDocument65 pagesFinal ResearchHarbrinder GurmNo ratings yet
- Alc Intra1 Questionnaire HypertensiveDocument5 pagesAlc Intra1 Questionnaire HypertensiveAndrea Blanca100% (1)
- Clinical Protocol for DVT ManagementDocument3 pagesClinical Protocol for DVT ManagementAnonymous cwRgUKv2MQ100% (1)
- 1 GloriosoDocument1 page1 GloriosoDARREN EDMARK100% (1)
- Research Paper PDFDocument11 pagesResearch Paper PDFevaNo ratings yet
- Lourlyn's Angels?Document27 pagesLourlyn's Angels?lovelove DayoNo ratings yet
- Chapter 1-3Document27 pagesChapter 1-3JellyAnnGomezNo ratings yet
- NCP ExamplesDocument1 pageNCP Examplesapi-316414872No ratings yet
- RRS at RRLDocument19 pagesRRS at RRLNicole MangosanNo ratings yet
- NCP For DRDocument1 pageNCP For DRvalencia222No ratings yet
- Physical Examination KoDocument8 pagesPhysical Examination KoJm Floyd R. MedenillaNo ratings yet
- Importance of Honesty in MedicineDocument3 pagesImportance of Honesty in MedicineSuiweng WongNo ratings yet
- Summary of Intravenous FluidDocument1 pageSummary of Intravenous FluidHshalalalaNo ratings yet
- Clinical TeachingDocument5 pagesClinical TeachingTobiDaNo ratings yet
- Course in The WardDocument1 pageCourse in The WardGeevee Naganag VentulaNo ratings yet
- Evidence-Based Nursing: I. Clinical QuestionDocument4 pagesEvidence-Based Nursing: I. Clinical QuestionRay Jorge MarmetoNo ratings yet
- Cap MR DDHDocument32 pagesCap MR DDHLovelle LopezNo ratings yet
- Nursing ESSAYDocument2 pagesNursing ESSAYMarsella Ayuthia AndiniNo ratings yet
- Case Analysis Group 1Document47 pagesCase Analysis Group 1bunso padillaNo ratings yet
- RRLDocument2 pagesRRLbunso padillaNo ratings yet
- Anatomy and Physiology-AppendicitisDocument3 pagesAnatomy and Physiology-AppendicitisMaria Socorro Sismundo DavidNo ratings yet
- Thyroid Lobectomy and IsthmusectomyDocument12 pagesThyroid Lobectomy and IsthmusectomyAgustina100% (1)
- Bea Case StudyDocument19 pagesBea Case StudyBea Flor Rapisura-PegadNo ratings yet
- Out Patient DepartmentDocument9 pagesOut Patient DepartmentBiway RegalaNo ratings yet
- GORDON'S FUNCTIONAL HEALTH PATTERNSDocument3 pagesGORDON'S FUNCTIONAL HEALTH PATTERNSGen RodriguezNo ratings yet
- Epidemiology and Pathophysiology of Colonic Diverticular DiseaseDocument8 pagesEpidemiology and Pathophysiology of Colonic Diverticular DiseaseAnonymous Hz5w55No ratings yet
- Diagnostic Test NursingDocument4 pagesDiagnostic Test NursingSuzette Rae TateNo ratings yet
- German MeaslesDocument8 pagesGerman MeaslesYdynn Parejas GavinaNo ratings yet
- Nursing and Patient Safety in The Operating Room: OriginalresearchDocument9 pagesNursing and Patient Safety in The Operating Room: OriginalresearchNovaa SeftianaNo ratings yet
- Nursing and Patient Safety in The Operating RoomDocument10 pagesNursing and Patient Safety in The Operating RoomJoe AbelloNo ratings yet
- Nursing Patient Safety in Or-With-Cover-Page-V2Document10 pagesNursing Patient Safety in Or-With-Cover-Page-V2gaynuwanketengNo ratings yet
- Rle Journal MackinnonDocument4 pagesRle Journal MackinnonAllyssa MackinnonNo ratings yet
- Dr. Namrata Misra Head of Bioinnovations at KIIT UniversityDocument1 pageDr. Namrata Misra Head of Bioinnovations at KIIT Universitymanisha maniNo ratings yet
- Nursing Care PlansDocument10 pagesNursing Care PlansGracie S. Vergara100% (1)
- Soal UTS Bahasa Inggris SMP Semester Genap Tahun Ajaran 2020Document5 pagesSoal UTS Bahasa Inggris SMP Semester Genap Tahun Ajaran 2020awan MustofaNo ratings yet
- Piping Material Classes GuideDocument98 pagesPiping Material Classes GuideLuis Pottozen VillanuevaNo ratings yet
- Allium CepaDocument90 pagesAllium CepaYosr Ahmed100% (3)
- Elem. Reading PracticeDocument10 pagesElem. Reading PracticeElissa Janquil RussellNo ratings yet
- Investigating Population Growth SimulationDocument11 pagesInvestigating Population Growth Simulationapi-3823725640% (3)
- B.Sc. (AGRICULTURE) HORTICULTURE SYLLABUSDocument31 pagesB.Sc. (AGRICULTURE) HORTICULTURE SYLLABUSgur jazzNo ratings yet
- Journalize The Following Transactions in The Journal Page Below. Add Explanations For The Transactions and Leave A Space Between EachDocument3 pagesJournalize The Following Transactions in The Journal Page Below. Add Explanations For The Transactions and Leave A Space Between EachTurkan Amirova100% (1)
- Owners Manual Water Mist PDFDocument6 pagesOwners Manual Water Mist PDFZeeNo ratings yet
- Formularium ApotekDocument12 pagesFormularium ApotekNurul Evi kurniatiNo ratings yet
- Hinduism Today April May June 2015Document43 pagesHinduism Today April May June 2015jpmahadevNo ratings yet
- CHAPTER3 Foundations of Individual BehaviorDocument32 pagesCHAPTER3 Foundations of Individual BehaviorLynoj AbangNo ratings yet
- M-LVDT: Microminiature Displacement SensorDocument2 pagesM-LVDT: Microminiature Displacement Sensormahdi mohammadiNo ratings yet
- FileDocument284 pagesFileJesse GarciaNo ratings yet
- fLOW CHART FOR WORKER'S ENTRYDocument2 pagesfLOW CHART FOR WORKER'S ENTRYshamshad ahamedNo ratings yet
- Nursing Plan of Care Concept Map - Immobility - Hip FractureDocument2 pagesNursing Plan of Care Concept Map - Immobility - Hip Fracturedarhuynh67% (6)
- Executive Order 000Document2 pagesExecutive Order 000Randell ManjarresNo ratings yet
- Hydrogeological Characterization of Karst Areas in NW VietnamDocument152 pagesHydrogeological Characterization of Karst Areas in NW VietnamCae Martins100% (1)
- Akshaya Trust NgoDocument24 pagesAkshaya Trust NgodushyantNo ratings yet
- Junayed - 19 39800 1Document11 pagesJunayed - 19 39800 1gurujeeNo ratings yet
- Family MedicineDocument156 pagesFamily MedicinedtriggNo ratings yet
- Nutrition During PregnancyDocument8 pagesNutrition During PregnancyHalliahNo ratings yet
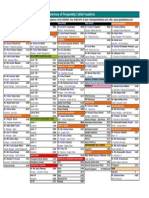
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- The Girls Center: 2023 Workout CalendarDocument17 pagesThe Girls Center: 2023 Workout Calendark4270621No ratings yet
- Retail Management PPT1Document14 pagesRetail Management PPT1Srilekha GubbalaNo ratings yet
- Cap 716 PDFDocument150 pagesCap 716 PDFjanhaviNo ratings yet
- Rreinforcement Pad Leak Test ProcedureDocument5 pagesRreinforcement Pad Leak Test ProcedureAmin Thabet100% (2)
- Quality Control Plan Static EquipmentDocument1 pageQuality Control Plan Static EquipmentdhasdjNo ratings yet
- How To Become A Coffee Aficionado: Tips & Tricks: Kate Macdonnell Brewing Updated: Feb 06 2023Document17 pagesHow To Become A Coffee Aficionado: Tips & Tricks: Kate Macdonnell Brewing Updated: Feb 06 2023sadenaikeNo ratings yet