Professional Documents
Culture Documents
Diabetes
Uploaded by
sshiffanaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetes
Uploaded by
sshiffanaCopyright:
Available Formats
DIABETES MELLITUS
BIOCHEMISTRY FOR U, CHENNAI http://biochemistryforu.googlepages.com/home V.VYTHEESHWARAN DIABETES MELLITUS Diabetes mellitus is a chronic disease due primarily to a disorder of carbohydrate metabolism, cause of which is deficiency or diminished effectiveness of insulin, resulting in hyperglycemia and glycosuria. May also cause secondary changes in metabolism of proteins, and lipids leading to grave consequences.
DIABETES STAGES There are 4 stages in diabetes: Pre-diabetics Suspected diabetes Chemical/Latent diabetes Overt diabetes Stages pre diabetics Suspected diabetes GIT normal abnormal FBS normal may be N Plasma insulin Symptoms normal N none symptom after stress Angiopathies + +
Chemical/Letent Diabetic Overt diabetic
abnormal Abnormal
N or
N or N or
unusual usual
++ +++ or ++++
DIABETES - TYPES There are three major forms of diabetes: Type I Diabetes (IDDM) (Juvenile onset) Type II Diabetes (NIDDM) (Maturity onset) Gestational Diabetes Secondary forms: Pancreatic Diabetes Hormonal Diabetes Iatrogenic Diabetes
DIABETES MELLITUS FACTORS Heredity Auto-immunity Infections Obesity Diet Insulin antagonism PATHOPHYSIOLOGY Pancreas is composed of cells scattered throughout called the islets of Langerhans Two types of cells are important to glucose control Alpha cells- produce glucagon Hormone that acts opposite of insulin Causes release of glucose from cell storage Beta cells- produce insulin Allows body cells to use and store carbohydrate, fat, and protien INSULIN Insulin is a protein made of 2 chains- alpha and beta Preproinsulin is produced initially Precursor molecule that is inactive Must be made smaller before becoming active Proinsulin Precursor that includes alpha and beta chains Also has a C-peptide chain C-peptide levels are used to measure rate that beta cells secrete insulin Insulin allows glucose to move into cells to make energy Liver is first major organ to be reached Promotes production and storage of glycogen (glycogenisis) Inhibits glycogen breakdown into glucose (glycogenolysis) Increases protein and lipid synthesis Inhibits tissue breakdown by inhibiting liver glycogenolysis (ketogenesis- converts fats to acids) & gluconeogenisis (conversion of proteins to glucose) In muscle, promotes protein and glycogen synthesis In fat cells, promotes triglyceride storage Pancreas secretes 40-50 units of insulin daily in two steps: Secreted at low levels during fasting ( basal insulin secretion Increased levels after eating (PP) An early burst of insulin occurs within 10 minutes of eating Then proceeds with increasing release as long as hyperglycemia is present GLUCOSE HOMEOSTASIS Glucose is main fuel for CNS Brain cannot make or store, therefore needs continuous supply Fatty acids can be used when glucose is not available ( triglycerides) Need 68-105 mg/dL to support brain Decreased levels of glucose, insulin release is stopped with glucagon released
GLUCOSE Glucagon causes release of glucose from liver Liver glucose is made thru glycogenolysis (glucogen to glucose) & Gluconeogenesis When liver glucose is not available, lypolysis occures ( breakdown of fat) OR Proteinlysis (breakdown of amino acids) ABSENCE OF INSULIN Insulin needed to move glucose into cells. Without insulin, body enters a state of breaking down fats and proteins. Glucose levels increase (hyperglycemia). DIABETES - TYPE I It results from primary beta cell destruction leading to absolute insulin deficiency. Also caused by genetic defects of beta cell; genetic defects in insulin action; other endocrine and exocrine dysfunctions; drug induced; other genetic syndromes Frequency-less Commences usually before 15 yrs of age. Frequency: Males > than Females. Onset-rapid and abrupt Speedy Progression to Keto-acidosis and coma Usually patients are thin and underweight Deficient Insulin: At first Juvenile diabetics produce more insulin than normal, but the beta-cells soon become exhausted and patient becomes "overt" diabetics with atrophied p-cells and practically no insulin . Plasma insulin- It is almost absent. No insulin response is shown to glucose load. Insulin therapy-is necessary for control of these cases. DIABETES TYPE II Frequency-more common. Occurs in middle aged individuals. More common in women. Onset is insidious Usually mild. Ketoacidosis is rare. Associated with obesity in2/3 of cases. Usually detected during routine check-up of urine. Beta cells respond normally. Relative insulin deficiency may be due to insulin antagonism. Plasma levels of insulin may be normal or raised. Oral hypoglycemic agents and diet control are useful in treatment. GESTATIONAL DIABETES Gestational diabetes mellitus (GDM) is defined as any degree of glucose intolerance with onset or first recognition during pregnancy. GDM SYMPTOMS Glycosuria. Elevated blood glucose levels. Usually appears between 24-28 weeks gestation. Degree of hyperglycemia is not as severe as in other types of diabetes.
SECONDARY DIABETES This condition is observed when diabetes occurs secondary to some diseases. Pancreatic diabetes: Pancreatitis Haemochromatosis Malignancy of Pancreas. Abnormal concentrations of antagonistic hormones Hyperthyroidism Hypercorticism: like Cushings syndrome Hyperpituitarism: like acromegaly Increased glucagon activity. Iatrogenic In genetically susceptible cases, may be precipitated by therapy like corticosteroids, thiazide diuretics. CLINICAL FEATURES AND BIOCHEMICAL CORRELATIONS Polyuria Polydypsia Polyphagia Weakness and fatigue Diabetic Ketoacidosis Hypercholesterolemia leading to atherosclerosis Weight loss Hemoconcentration- related to dehydration Hypovolemia- decreased blood volume Hyperviscosity thick concentrated blood Hypoperfusion- decreased circulation Hypokalemia and Hyponatremia Kussmaul respirations
Polyuria: Frequent and excessive urination Osmotic diuresis caused by excess glucose in urine Water loss can be severe along with sodium, chloride, and potassium Polydipsia: Excessive thirst associated with dehyration Polyphagia: Cells do not receive glucose leading to starvation which triggers excessive eating Weakness and fatigue Due to lack of glucose available for ATP formation. Weight loss Catabolism of lipids and proteins as a part of gluconeogenesis Diabetic Ketoacidosis DKA results in altered lipid metabolism. increased concentrations of total lipids, cholesterol, triglycerides, and free fatty acids. free fatty acids are shunted into ketone body formation due to lack of insulin; the rate of formation exceeds the capacity for their peripheral utilization and renal excretion leading to accumulation of ketoacids, and therefore metabolic acidosis.
Hypercholesterolemia & Atherosclerosis Abnormal lipid metabolism leading to FFA and cholesterol biosynthesis. Cholesterol deposition - lead pipe arteries Kussmaul respirations: Excess acids cause increased H+ and CO2 levels Stimulate brain to increase rate and depth of respirations to excrete acid and carbon dioxide Acetone is exhaled thus breath has fruity odor Ultimately, pH will drop Hypokalemia and Hyponatremia Lack of insulin causes depletion of potassium and sodium CHRONIC COMPLICATIONS Blood vessels changes Macrovascular: Coronary heart disease, cerebrovascular accidents; & peripheral vascular disease Major risk factor for CAD, MI Microvascular: Nephropathy (kidney dysfunction); neruopathy (nerve dysfunction); & retinopathy (vision problems) Blindness is 25 times more common Microaneurysms Neovascularization- new blood vessels but thin, fragile and bleed easily Male erectile dysfunction (ED) DIABETIC RETINOPATHY Diabetes results in changes in veins, arteries and capillaries in the body. Risk of developing diabetic retinopathy: damage occurs to the fragile blood vessels inside the retina. Could develop cataracts (clouding of the naturally clear lens in the eye). May develop glaucoma (a disease of the optic nerve). 2 Forms Non proliferative Diabetic Retinopathy (NPDR) and Proliferative Diabetic Retinopathy (PDR). NPDR Early stage diabetic retinopathy Hard exudates on the central retina (macula). Microaneurysms (small bulges in blood vessels of the retina that often leak fluid). Retinal hemorrhages (tiny spots of blood that leak into the retina). Macular edema (swelling/thickening of macula). Macular ischemia (closing of small blood vessels/capillaries). Retina showing NPDR
PDR Later stage diabetic retinopathy Vitreous hemorrhage (new, abnormal blood vessels bleed into vitreous gel in center of eye, preventing light rays from reaching the retina).
Traction retinal detachment (new, abnormal blood vessels begin to shrink and tug on retina; may cause retina to detach). Neovascular glaucoma (neovascularization occurs in the iris, causing pressure to build up in the eye, damaging the optic nerve). Retina showing PDR DIABETIC NEPHROPATHY Diabetic nephropathy (nephropatia diabetica), also known as Kimmelstiel- Wilson syndrome and intercapillary glomerulonephritis. It is a progressive kidney disease caused by angiopathy of capillaries in the kidney glomeruli. Characterized by nodular glomerulosclerosis. DIABETIC NEPHROPATHY Stage 1: Hyperfiltration, or an increase in glomerular filtration rate (GFR) occurs. Kidneys increase in size. Stage 2: Glomeruli begin to show damage and microalbuminurea occurs. Stage 3: Albumin excretion rate (AER) exceeds 200 micrograms/minute, and blood levels of creatinine and urea-nitrogen rise. Blood pressure may rise during this stage. Stage 4: GFR decreases to less than 75 ml/min, large amounts of protein pass into the urine, and high blood pressure almost always occurs. Levels of creatinine and urea-nitrogen in the blood rise further. Stage 5: Kidney failure, or end stage renal disease (ESRD). GFR is less than 10 ml/min. The average length of time to progress from Stage 1 to Stage 4 kidney disease is 17 years for a person with type 1 diabetes. The average length of time to progress to Stage 5, kidney failure, is 23 years. HYPERGLYCEMIC- HYPEROSMOLAR-NONKETOTIC SYNDROME AND COMA Increased blood osmolarity caused by hyperglycemia Absence of ketosis and higher blood glucose levels & blood osmolarity (>800mg/dL) (44.5 mmol/L) Other manifestations are more severe HHNS MI, sepsis, pancreatitis, stroke, some drugs may cause HHNS Clients may have seizures or reversible paralysis Related to residual insulin secretion: client secretes just enough insulin to prevent ketoacidosis, but not hyperglycemia Profound diuresis with e-lyte imbalance Decreased kidney perfusion leads to decreased urine output leading to decreased glucose in urine DIABETIC NEUROPATHY AND DIABETIC FOOT Neuropathy Sensory Motor autonomic Regulates sweating and perfusion to the limb Loss of autonomic control inhibits thermoregulatory function and sweating Result is dry, scaly and stiff skin that is prone to cracking and allows a portal of entry for bacteria DIABETIC FOOT Loss of protective sensation Starts distally and migrates proximally in stocking distribution Large fibre loss light touch and proprioception
Small fibre loss pain and temperature Usually a combination of the two. Mild form of diabetic foot Charcot foot Mostly affects forefoot ulceration Intrinsic muscle wasting claw toes Equinous contracture Two mechanisms of Ulceration Unacceptable stress few times rock in shoe, glass, burn Acceptable or moderate stress repeatedly Improper shoe ware deformity DIABETIC FOOT Wagners Classification 2. Intact skin (impending ulcer) 3. Superficial 4. Deep to tendon bone or ligament 5. Osteomyelitis (Bone marrow inflammation) 6. Gangrene of toes or forefoot 7. Gangrene of entire foot TREATMENT PROTOCOLS
METABOLIC CHANGES IN DIABETES MELLITUS
LAB DIAGNOSTICS Urine tests: Ketones Renal function Glucose Blood tests: Fasting blood glucose test Oral glucose tolerance test Glycosylated hemoglobin assays Glycosylated serum proteins and albumin URINE TESTS Ketones: Waste products of fat metabolism Presence in urine may indicate pending ketoacidosis Renal function: Urine protein without renal symptoms may indicate microvascular changes Albumin at 30-3000 mg/hr indicates too much protein in urine (microalbuminemia) Creatinine clearance tests Glucose: Blood glucose can be measured indirectly through urine BLOOD TESTS Fasting blood glucose: Obtain blood thru venipuncture Fast for 8 hours Draw before Rx given; >126mg/dL X 2 Oral glucose tolerance: Most sensitive test, but not routinely used Drinks beverage with 75 g of glucose; blood samples are drawn at 30 min intervals for 2 hours. >200 mg/dL at 120 minutes Glycosylated hemoglobin assays: Blood glucose attaches to hemoglobin Higher the glucose over time, > glycosyolated hemoglobin Good indicator of average blood glucose levels (HbA1c) Average glucose over last 120 days-life span of RBCs Glycosylated serum proteins and albumim: Like hemoglobin, serum proteins and albumin become satuated with glucose over time Turnover rate for proteins and albumin is 14 days, therefore assesses glucose over shorter period of time DIABETES MANAGEMENT -MEALS MUST BE INDIVIDUALIZED NO SUCH THING AS DIABETIC DIET PORTION CONTROL IS THE KEY Goals include: Keep BS and HgbA1c normal Optimal lipid levels
Optimal BP Ensure adequate calories Preventing complications Improve overall health Facilitate healthy eating habits Meet nutritional and psychological needs Provide self management education May help to facilitate moderate weight loss if at risk for complications of obesity Day to day consistency in timing and amount helps control blood glucose Protein, carbohydrates, and fats must be consumed in appropriate amounts Protein- 15-20% of total daily calories in clients with normal renal function (reduce to9 10% in renal dysfunction) Fat- <10% saturated fats; up to 10% in polyunsaturated fats Carbohydrates- emphasis in on total amount of CHO, not source High fiber improve carbohydrate metabolism and lower cholesterol (20-35 g of fiber per day) Increase fluid intake with fiber Nonnutritive sweeteners: Saccharin Aspartame Acesulfame K Sucralose Fat replacers: < 5 g of CHO per meal or < 20 calories Limit to 3 servings per day Excess calories from any source are stored as adipose tissue and the storage capacity is unlimited Alcohol: Moderate use if ok if diabetes is contolled; at risk for hypoglycemia so ingest with meals Exchange system: no one size fits all Based on 3 food groups Individualized for each meal CHO counting Focus on total CHO amounts CHO controls blood glucose levels 1 unit of rapid-acting insulin for each 15 g of CHO Special considerations Type I- spread CHO over 3 meals; avoid gaining weight Type II- reduce calories eaten and increase calories expended; 3 meals with snacks MEDICATIONS All medications must be used along with diet, exercise and stress management Two types to control diabetes: Antidiabetic agents Insulin Oral therapy: prescribed after dietary control has been proven insufficient or if the client is highly symptomatic Classifications:
Sulfonylureas Meglitnide analogs Biguanides Alpha-glucosidse inhibitors Thiazolidinedione antidiabetic agents MEDICATIONS: INSULIN Insulin therapy is needed for Type I and many Type II diabetics Many types of insulin Dose varies but between 0.5-1 unit/kg/day Safety is issue for elderly patients, vision, mobility, coordination, and memory deficits INSULIN Types of insulin: Obtained for animal sources such as beef or pork pancreas, combined, synthetic human and semi- synthetic. There are differences in strength and onset of action between human and animal insulins Human is more rapid acting, shorter peak action, and shorter duration Human insulin is preferred during pregnancy or with clients with allergies or resistance to animal sources Protocols: Single daily: Two-dose: 2/3 before breakfast; 1/3 in evening Three-dose: breakfast, evening, bedtime Four-dose: before meals, bedtime New technologies: Insulin pumps: Inject continuous basal doses of insulin with increased doses at meals. Implanted insulin pumps: implanted into peritoneal cavity where blood supply absorbs insulin. Needleless devices: ultrathin liquid is forced under the skin with high pressure. Pen-type injectors: more precise smaller doses, easy to carry and use. Inhaled insulin: under development; pellet that is vaporized in an inhaler (like spiriva).
Photograph reproduced with permission of manufacturer. SUMMARY There is nothing inevitable about the complications of diabetes. However, the evidence is overwhelming that good control does count. Morbidity and mortality can be reduced. Insulin administration should mimic nature Natures way is basal insulin 24 hrs. a day. Insulin glargine or detemir can supply the basal with one injection per day. Assessment tools include Self Monitoring of Blood Glucose and HbA1C. Targets should be established for each of these for each patients within the national guidelines. When targets are not reached the help of a specialist should be sought.
You might also like
- HPN and DM LectureDocument23 pagesHPN and DM Lectureivy rose duhilagNo ratings yet
- Nursing Care of PT With DiabetesDocument71 pagesNursing Care of PT With DiabetesEricka Lj Robles DimaculanganNo ratings yet
- Kindergarten Physical Education LessonDocument7 pagesKindergarten Physical Education Lessonapi-185987237No ratings yet
- Diabetes MellitusDocument59 pagesDiabetes Mellitusuzzal ahmedNo ratings yet
- Diabetes MellitusDocument59 pagesDiabetes Mellituslailatul rofiahNo ratings yet
- Diabetes MellitusDocument60 pagesDiabetes MellitusVytheeshwaran Vedagiri96% (26)
- Dka (Picucourse)Document33 pagesDka (Picucourse)surasuarezlopezNo ratings yet
- Diabetes MellitusDocument9 pagesDiabetes MellitusM. Joyce100% (2)
- Diabetic Ketoacidosis in ChildrenDocument39 pagesDiabetic Ketoacidosis in ChildrenRichard SiahaanNo ratings yet
- L11 Diabetes MellitusDocument61 pagesL11 Diabetes MellitusYosra —No ratings yet
- Diabetic Emergencies and ManagementDocument41 pagesDiabetic Emergencies and ManagementNali peterNo ratings yet
- DiabetesDocument32 pagesDiabetesaneeshajaiswalNo ratings yet
- Lecture 28 - Pathology of DiabetesDocument34 pagesLecture 28 - Pathology of Diabetesapi-3703352100% (4)
- Askep DMDocument78 pagesAskep DMSiti SangadahNo ratings yet
- Diabetes MellitusDocument52 pagesDiabetes MellitusMervis masatunyaNo ratings yet
- Diabetic EmergenciesDocument41 pagesDiabetic EmergenciesYuNa YoshinoyaNo ratings yet
- Diabetes MellitusDocument29 pagesDiabetes MellitusSyed MaazNo ratings yet
- DIABETISDocument52 pagesDIABETISNeeraja M SureshNo ratings yet
- COMPICATION of DMDocument42 pagesCOMPICATION of DMSaif AliNo ratings yet
- Medical EmergenciesDocument12 pagesMedical EmergenciesBSN 2 - Sasis, Rusmaryte C.No ratings yet
- Diabetic Coma in Type 2 DiabetesDocument4 pagesDiabetic Coma in Type 2 DiabetesGilda Ditya AsmaraNo ratings yet
- Presentation 1Document9 pagesPresentation 1p1awh1786No ratings yet
- Disease Manifestations and PathologyDocument34 pagesDisease Manifestations and PathologyAnjali TakkeNo ratings yet
- Endo - DMDocument24 pagesEndo - DMdoctorrfarrukhNo ratings yet
- Diabetes Mellitus: - ClassificationDocument22 pagesDiabetes Mellitus: - ClassificationFernando Junior Parra UchasaraNo ratings yet
- Diabetes MellitusDocument62 pagesDiabetes MellitusPrabhuswamyChowdiah100% (1)
- PuneetDocument11 pagesPuneetRudraksha pratap singhNo ratings yet
- Diabetes Mellitus.U.iiDocument38 pagesDiabetes Mellitus.U.iitamtamtamtama0No ratings yet
- Diabetes MellitusDocument48 pagesDiabetes MellitusDhruvil GadhiyaNo ratings yet
- Diabetes Mellitus: Prepared by Divya Bhusal B.SC - Nursing 3 YearDocument43 pagesDiabetes Mellitus: Prepared by Divya Bhusal B.SC - Nursing 3 YearSristi LamsalNo ratings yet
- Acute Complication of DMDocument41 pagesAcute Complication of DMWhite Crime100% (1)
- Module 08 - Endocrine DisordersDocument43 pagesModule 08 - Endocrine DisordersKarina LojaNo ratings yet
- Diabetic Ketoacidosis Management: Heidi Chamberlain Shea, MDDocument29 pagesDiabetic Ketoacidosis Management: Heidi Chamberlain Shea, MDSiti RahmahNo ratings yet
- Chapter 4 Carbohydrate DisorderDocument26 pagesChapter 4 Carbohydrate DisorderNida RidzuanNo ratings yet
- Diabetes Younes Ferwana Mohamed MehgizDocument43 pagesDiabetes Younes Ferwana Mohamed MehgizHakim oğluNo ratings yet
- Complications DM FinalDocument57 pagesComplications DM FinalBarbie GirlNo ratings yet
- Physical Evaluation I (Dent 5121) : Endocrine System: Diabetes MellitusDocument47 pagesPhysical Evaluation I (Dent 5121) : Endocrine System: Diabetes MellitusShosoo ShooshoNo ratings yet
- Metabolic EmergenciesDocument53 pagesMetabolic EmergenciesWengel Redkiss100% (1)
- EndokrinologiDocument28 pagesEndokrinologiChris LaurenNo ratings yet
- Assessment - and - Management - of - Patients - With - Diabetes - Mellitus (1) FINALDocument80 pagesAssessment - and - Management - of - Patients - With - Diabetes - Mellitus (1) FINALAMIT MODWALNo ratings yet
- WEEK 15 DiabetesDocument68 pagesWEEK 15 DiabetesEditha LucasNo ratings yet
- Diabetic Ketoacidosis (DKA) VS. Hyperosmolar Hyperglycemic Syndrome (HHS)Document5 pagesDiabetic Ketoacidosis (DKA) VS. Hyperosmolar Hyperglycemic Syndrome (HHS)MrRightNo ratings yet
- Week4 EndocrineDocument84 pagesWeek4 EndocrineriverabeanicoNo ratings yet
- Nursing Care of Patients With Diabetes MellitusDocument11 pagesNursing Care of Patients With Diabetes MellitusMarcus, RN100% (32)
- Endocrine & Metabolic DisordersDocument38 pagesEndocrine & Metabolic DisordersBala UrmarNo ratings yet
- Type 1 Diabetes Mellitus Nael HernandezDocument15 pagesType 1 Diabetes Mellitus Nael HernandezShermayne Mallapre HernandezNo ratings yet
- Week 7 Diabetes MellitusDocument34 pagesWeek 7 Diabetes MellitusHERLIN HOBAYANNo ratings yet
- DM FinalDocument58 pagesDM FinalMalueth AnguiNo ratings yet
- Diabetes and Diabetic KetoacidosisDocument11 pagesDiabetes and Diabetic KetoacidosisPayoja RajNo ratings yet
- Clinical SignificanceDocument31 pagesClinical Significancejav israelNo ratings yet
- Diabetes MellitusDocument24 pagesDiabetes MellitusAdi Prabowo SyamsNo ratings yet
- Endocrine Emergencies: Lynn K. Wittwer, MD MPD Clark County EMSDocument37 pagesEndocrine Emergencies: Lynn K. Wittwer, MD MPD Clark County EMSSyahril FauziNo ratings yet
- REVALIDADocument53 pagesREVALIDAMercy Anne EcatNo ratings yet
- Diabetes-Cho 2023 3rd Yr.Document37 pagesDiabetes-Cho 2023 3rd Yr.abdulrahmanbelewa96No ratings yet
- REVALIDADocument53 pagesREVALIDAMercy Anne EcatNo ratings yet
- Diabetes Mellitus: Pediatric Critical Care Medicine Emory University Children's Healthcare of AtlantaDocument46 pagesDiabetes Mellitus: Pediatric Critical Care Medicine Emory University Children's Healthcare of AtlantaAbdulkarim Mohamed AbdallaNo ratings yet
- Diabetes KetoacidosisDocument27 pagesDiabetes Ketoacidosisyose rizal sinagaNo ratings yet
- Acute Complications of DMDocument57 pagesAcute Complications of DMMalueth AnguiNo ratings yet
- Diabetic Recipes for One and TwoFrom EverandDiabetic Recipes for One and TwoRating: 3 out of 5 stars3/5 (1)
- Diabetic Cooking for One and TwoFrom EverandDiabetic Cooking for One and TwoRating: 3 out of 5 stars3/5 (1)
- Low Blood Sugar: The Nutritional Plan to Overcome Hypoglycaemia, with 60 RecipesFrom EverandLow Blood Sugar: The Nutritional Plan to Overcome Hypoglycaemia, with 60 RecipesNo ratings yet
- Nutrition For Liver Gallbladder and Pancreas DiseasesDocument39 pagesNutrition For Liver Gallbladder and Pancreas DiseasesMaricar Car CartallaNo ratings yet
- Clinical Applied Anatomy in Wound CareDocument18 pagesClinical Applied Anatomy in Wound CareKlinik Komuniti Perwira100% (2)
- Cmca Activity 1 AliamenDocument5 pagesCmca Activity 1 AliamenJasmine AliamenNo ratings yet
- Physiotherapy For Vascular PatientDocument44 pagesPhysiotherapy For Vascular PatientHaengbokaeyo Hua Min100% (4)
- The Right To Die: Pre-ReadingDocument8 pagesThe Right To Die: Pre-ReadingGiovanni EscobarNo ratings yet
- Jesse Smith Letter of ReccDocument1 pageJesse Smith Letter of Reccapi-510425013No ratings yet
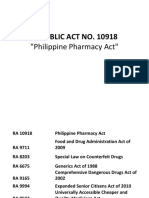
- PharmacyDocument78 pagesPharmacyGelie BundocNo ratings yet
- Lesson 1 Physical Fitness and Related ActivitiesDocument31 pagesLesson 1 Physical Fitness and Related ActivitiesKaiNo ratings yet
- Ijshr0038 PDFDocument9 pagesIjshr0038 PDFNilakshi Barik MandalNo ratings yet
- Introduction To Soya BeanDocument6 pagesIntroduction To Soya BeanMisbah FatimahNo ratings yet
- g1fm Ims Obj 001 Ims ObjectivesDocument3 pagesg1fm Ims Obj 001 Ims ObjectivesIan DañgananNo ratings yet
- Attending Physician Statement (APS) - TPD - FamilyDocument3 pagesAttending Physician Statement (APS) - TPD - FamilyTaufik Hameed SultanNo ratings yet
- OHS-PR-09-03-F02 RISK ASSESSMENT For INSTALLATION OF WALL MOUNTED JIB CRANEDocument21 pagesOHS-PR-09-03-F02 RISK ASSESSMENT For INSTALLATION OF WALL MOUNTED JIB CRANEmohammed tofiqNo ratings yet
- Handout 2: Identifying Hazards and Risk Control in The Café: Step 1: Rest Step 2: Ice For Step 3: Step 4: ElevateDocument2 pagesHandout 2: Identifying Hazards and Risk Control in The Café: Step 1: Rest Step 2: Ice For Step 3: Step 4: ElevateSneha DhamijaNo ratings yet
- Activity 26 Assessment and Care of Antenatal Woman Ante Natal Case Record - 2Document5 pagesActivity 26 Assessment and Care of Antenatal Woman Ante Natal Case Record - 2A J FathimaNo ratings yet
- The Dangers of Sitting - Why Sitting Is The New Smoking - Better Health ChannelDocument10 pagesThe Dangers of Sitting - Why Sitting Is The New Smoking - Better Health ChannelTHE PRATHAM SRIVASTAVA.No ratings yet
- An Overview of The Role of Nurses and Midwives in Leadership and Management in EuropeDocument44 pagesAn Overview of The Role of Nurses and Midwives in Leadership and Management in EuropeTCNo ratings yet
- What I Need To Know: Pe10Pf-Iva-H-39Document11 pagesWhat I Need To Know: Pe10Pf-Iva-H-39Ruby BationNo ratings yet
- Kesh Dant NakhDocument6 pagesKesh Dant Nakhdouble slit photon50% (2)
- Chapter 4. Ergonomics Hazards and Risks ManagementDocument46 pagesChapter 4. Ergonomics Hazards and Risks Managementmich abi100% (1)
- Annex B. School Level Report On The 3rd Quarter NSEDDocument3 pagesAnnex B. School Level Report On The 3rd Quarter NSEDMaria Claret alcazarNo ratings yet
- Sabrina ManigoDocument2 pagesSabrina ManigoCOREY RICHNo ratings yet
- Snapps PDFDocument1 pageSnapps PDFPatty Rivera100% (1)
- Overview of Health Informatics: Lesson 4Document8 pagesOverview of Health Informatics: Lesson 4Jennifer Ledesma-PidoNo ratings yet
- Health and Safety FlowDocument6 pagesHealth and Safety Flowzaki0304No ratings yet
- Advanced Herd Health Management, Sanitation and HygieneDocument28 pagesAdvanced Herd Health Management, Sanitation and Hygienejane entunaNo ratings yet
- 2012 Costs Fact Sheet Version Alzheimers AssociationDocument2 pages2012 Costs Fact Sheet Version Alzheimers AssociationynottripNo ratings yet
- Nursing Home Abuse - A Rising Threat in The USDocument8 pagesNursing Home Abuse - A Rising Threat in The USLezDo techmed LLCNo ratings yet
- Drug Study OxytocinDocument3 pagesDrug Study OxytocinSheena Marie M. TarleNo ratings yet