Professional Documents
Culture Documents
Gap PCR
Uploaded by
vishankguptaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gap PCR
Uploaded by
vishankguptaCopyright:
Available Formats
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
PROTOCOL
Gap - PCR
Gap-PCR
Principle
Gene deletion mutations in the -globin gene cluster may be detected by PCR using
two primers complimentary to the sense and antisense strand in the DNA regions that
flank the deletion. For small deletions of less than one kilobase, the primer pair will
generate two products, the smaller fragment arising from the deletion allele. For large
deletions, the distance between the two flanking primers is too great to amplify the
normal allele and product is only obtained from the deletion allele. In these cases the
normal allele is detected by amplifying across one of the breakpoints, using a primer
complimentary to the deleted sequence and one complimentary to the flanking DNA.
Gap-PCR is used for to diagnose some -thlassaemia deletions, HPFH deletions, -
thalassaemia deletions (Table 5.2) and also the triple a-gene locus generated by the
3.7kb single -gene deletion [5]. A typical gap-PCR test is illustrated in Figure 5.10
and 5.11. For the diagnosis of -thalassaemia, the primers can now be multiplexed.
The 3.7kb and 4.2kb
+
-thalassaemia deletions can be detected in one assay (table
5.9), the --
MED
and -()
20.5
-thalassaemia deletions in one assay (table 5.10) and the
3 Southeast Asian
-thalassaemia deletions in one assay (Table 5.11). The protocols
used in the Oxford laboratory for the multiplexing of these primers are given in
Tables 5.9-5.11, but it should be noted that the quantity of each primer pair relative to
the others may need adjustment to gain optimum amplification of all the products.
PCR diagnosis of the triple -gene (anti 3.7 allele) requires two separate assays
section
Molecular diagnosis procedures Diagnosis of known mutations
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
(Tables 5.12 & 5.13). The presence of the allele is diagnosed from a comparison of
the results of each assay run side by side and the genotype of the DNA sample can be
deduced (Table 5.14) in most instances.
Table 5.2. Thalassaemia deletion mutations which have been diagnosed by gap-PCR
o
-thalassaemia
+
-thalassaemia
o
-thalassaemia
()
o
-thalassaemia
(
A
)
o
-thalassaemia
HPFH
--
SEA
--
MED
-()
20.5
--
FIL
--
THAI
-
3.7
-
4.2
290 bp deletion
532 bp deletion
619 bp deletion
1393 bp deletion
1605 bp deletion
3.5 kb deletion
10.3 kb deletion
45 kb deletion
Hb Lepore
Spanish
Sicilian
Vietnamese
Macedonian/Turkish
Indian
Chinese
HPFH1 (African)
HPFH2 (Ghanaian)
HPFH3 (Indian)
Hb Kenya
[6]
[6]
[6]
[8,9]
[8.9]
[7]
[7]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[20]
[20]
[20]
[20]
[20]
[20]
[20]
[20]
[20]
[20]
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
Method
1. Set up the reaction mixture to a final volume of 22 l into a 0.5 ml tube with
the following components as required: 1 l genomic DNA (100 ng/l) (1 l of
forward primer - flanking sequence (10 pmol/l), 1 l reverse primer -
flanking sequence (10 pmol/l),1 l of primer - deleted sequence (10
pmol/l), 1 l of primer - inverted sequence (10 pmol/l), 2.5 l of 1.25 mM
(dNTP mixture), 2.3 l of 10x Gap PCR buffer as recommended for the
primers in the original reference (see Table 5.2) and below.
2. The buffer recommended for the -thalassaemia primers is 750 mM Tris-HCl
pH 8.8, 200 mM (NH
4
)
2
SO
4
, 0.1% Tween 20). The buffer for the -
thalassaemia primers should also contains 0.5 M betaine and 0.5% DMSO
(this can be achieved by adding 2.5 l of 5 M betaine and 1.25 l 10%
DMSO).
3. Make up all reactions to a final volume of 22 l by adding sterile dH
2
O.
4. Overlay with 25 l of mineral oil.
5. Prepare enzyme mixture: 0.2 l reaction buffer (10x), 0.1 l AmpliTaq
(5U/l) (PE Biosystems) for the -gene primers, 0.1 l Platinum Taq (5U/l)
(Invitrogen) for the -gene primers, and 2.7 l sterile dH
2
O, to make 3 l.
6. Mix enzyme mixture and hold on ice.
7. Place reaction mixtures in thermal cycler and perform one cycle as follows,
adding 3 l of the enzyme mix after 2 minutes of the 94
o
C denaturation step:
4 min at 94
o
C/ 1 min at 55-65
o
C (as recommended)/ 1.5 min at 72
o
C
8. Continue for 33 cycles with the following steps per cycle: 1 min at 94
o
C/1
min at 55-65
o
C (as recommended in the published references or in tables 5.9-
5.13)/1.5 min at 72
o
C
9. Finish with one cycle as follow: 1 min at 94
o
C/1 min at 55-65
o
C (as
recommended)/10 min at 72
o
C.
10. Hold at 15
o
C until gel electrophoresis.
11. Remove tubes from thermal cycler. Add 5 l of blue dye, mix and centrifuge.
12. Depending on expected product sizes, load a 20 l aliquot onto a 1-3%
agarose gel and run at 100 V for 45 min to 2 hrs in 1x Tris-borate-EDTA
buffer (TBE).
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
13. Stain gel in ethidium bromide solution (0.5 g/ml) for 15-30 minutes,
visualise bands on a UV light box (312 nm) and photograph with an electronic
camera system or a Polaroid CU-5 camera fitted with an orange filter (e.g.
Wratten 22A). For guidance re interpretation see notes 6,7 and 8.
Materials
a) DNTPs: Add together 50 l of a 100 mM solution of each dNTP (as
purchased) and 3.8 ml of distilled water. The 1.25 mM dNTP stock solution
should be stored in frozen aliquots.
b) 10x Gap PCR reaction buffer (composition varies according to primers used)
see methods and Table 2
c) Betaine (Sigma-Aldrich Chemical Co Ltd, England)
d) Mineral Oil to overlay PCR reactions
e) PCR primers: dilute aliquots of primer stock solutions to make a working
solution of 1 OD unit/ml and store frozen.
f) Ammonium sulphate buffer: 75 mM Tris-HCl (pH 9.0), 20 mM (NH
4
)
2
SO
4
,
2.0 mM MgCl
2
, 0.01% Tween 20, 10% DMSO, 10 mM -mercaptoethanol
(all final concentrations).
g) Taq polymerases and 10x Taq buffers: in my laboratory are as follows,
AmpliTaq Gold (PE Biosystems) works best for ARMS-PCR/RE digestion
assays and Platinum Taq (Gibco Life Technologies) for gap-PCR.
h) Tris-borate -EDTA (TBE) buffer : 89 mM Tris-borate, 89 mM boric acid, 10
mM EDTA, pH 8.0.
i) Blue running dye (15% ficoll/0.05% bromophenol blue).
j) UV transilluminator and Polaroid camera, or UV electronic camera system
k) 0.5 g/l Ethidium bromide
Multiplex Gap-PCR
Specific primer details etc are listed below for the multiplex diagnosis of the common
-thalassaemia genotypes and the triplicated -globin allele. Figures 5.10 and 5.11
show example results all the common -thalassaemia geneotypes.
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
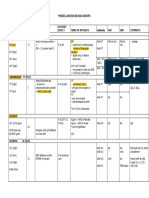
1. Multiplex PCR protocol for the diagnosis of
3.7
and
4.2
deletions.
A) Primer sequences
primer description sequence Annealing temp
0
C
1 2/3.7-F CCCCTCGCCAAGTCCACCC 64
2 3.7/20.5-R AAAGCACTCTAGGGTCCAGCG 64
3 2-R AGACCAGGAAGGGCCGGTG 64
4 4.2-R CCCGTTGGATCTTCTCATTTCCC 64
5 4.2-F GGTTTACCCATGTGGTGCCTC 64
B) PCR reaction mix
component
l
2/3.7-F (10 M)
1.0
2-R (10 M)
0.25
2/20.5-R (10 M)
1.0
4.2-F (10 M)
1.0
4.2-R (10 M)
1.5
10x buffer (750 mM Tris-HCl pH 8.8,
200 mM (NH
4
)
2
SO
4
, 0.1% Tween 20)
2.5
25 mM MgCl
2
1.5
dNTPs (1 mM)
5.0
Betaine (5 M)
3.75
DMSO (10%)
1.25
Platinum Taq (5 units /l)
0.1
DNA template (100 ng/l)
1.0
Water
5.2
C) Gel electrophoresis conditions
Run PCR products out on 1.5% (1:1 Nusieve:agarose ) gel for 2-3 hours
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
D) Interpretation of results
PCR Fragment size (bp) Genotype Product of primers
2020
+
-thalassaemia: -
3.7
1 + 2
1800 Normal () 1 + 3
1628
+
-thalassaemia: -
4.2
4 + 5
2. Multiplex PCR protocol for the diagnosis of the --
MED
and -()
20.5
deletions.
A) Primer sequences
primer name sequence Annealing
temp
0
C
1 MED(F) CGATGAGAACATAGTGAGCAGAATTGCAGG 60
2 MED(R) ACGCCGACGTTGCTGCCCAGCTTCTTCCAC 60
3 SEA(F) CTCTGTGTTCTCAGTATTGGAGGGAAGGAG 60
4 SEA(N) TGAAGAGCCTGCAGGACCAGGTCAGTGACCG 60
5 -()
20.5
(F) GGGCAAGCTGGTGGTGTTACACAGCAACTC 60
6 -()
20.5
(R)
CCACGCCCATGCCTGGCACGTTTGCTGACG 60
B) PCR reaction mix
component l
SEA(F) (10 M) 1.0
SEA(N) (10 M) 0.5
MED(F) (10 M) 0.4
MED(R) (10 M) 0.4
-()
20.5
(F) (10 M) 0.4
-()
20.5
(R) (10 M) 0.4
10x buffer (750 mM Tris-HCl pH 8.8,
200 mM (NH
4
)
2
SO
4
, 0.1% Tween 20)
2.5
25 mM MgCl
2
1.5
dNTPs (1 mM) 4.0
Betaine (5 M) 3.75
DMSO (10%) 1.25
Platinum Taq (5 units /l) 0.1
DNA template (100 ng/l) 1.0
Water 6.2
C) Gel electrophoresis conditions
Run PCR products out on 2% (1:1 Nusieve:agarose ) gel for 1-1.5 hours
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
D) Interpretation of results
PCR Fragment size (bp) Genotype Product of primers
1175
0
-thalassaemia: -()
20.5
5 + 6
1010 Normal () 3 + 4
875
+
-thalassaemia: --
MED
1 + 2
3. Multiplex PCR protocol for the diagnosis of the --
SEA
/ --
FIL
/ --
THAI
0
-
thalassaemia deletions.
A) Primer sequences
primer name Sequence Annealing
temp
0
C
1 FIL (F) AAGAGAATAAACCACCCAATTTTTAAATGGGCA 60
2 FIL (R) GAGATAATAACCTTTATCTGCCACATGTAGCAA 60
3 SEA(F) CTCTGTGTTCTCAGTATTGGAGGGAAGGAG 60
4 SEA(N) TGAAGAGCCTGCAGGACCAGGTCAGTGACCG 60
5 SEA(R) ATATATGGGTCTGGAAGTGTATCCCTCCCA 60
6 THAI(F) CACGAGTAAAACATCAAGTACACTCCAGCC 60
7 THAI(R) TGGATCTGCACCTCTGGGTAGGTTCTCTACC 60
B) PCR reaction mix
component l
SEA(F) (10 M) 2.0
SEA(N) (10 M) 1.0
SEA(R) (10 M) 1.0
FIL (F) (10 M) 4.0
FIL (R) (10 M) 4.0
THAI (F) (10 M) 1.0
THAI (R) (10 M) 1.0
10x buffer (750 mM Tris-HCl pH 8.8,
200 mM (NH
4
)
2
SO
4
, 0.1% Tween 20)
2.5
25 mM MgCl
2
1.5
dNTPs (1 mM) 4.0
Betaine (5 M) 3.75
DMSO (10%) 1.25
Platinum Taq (5 units /l) 0.1
DNA template (100 ng/l) 1.0
Water 0.65
C) Gel electrophoresis conditions
Run PCR products out on 1.5% (1:1 Nusieve:agarose ) gel for 2 hours
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
D) Interpretation of results
PCR Fragment size (bp) Genotype Product of primers
1010 Normal () 3 + 4
660
+
-thalassaemia: --
SEA
3 + 5
550
+
-thalassaemia: --
FIL
1 + 2
495
+
-thalassaemia: --
THAI
6 + 7
4.1 PCR protocol for the diagnosis of the (anti 3.7) allele: reaction mix 1
A) Primer sequences
primer description sequence Annealing
temp
0
C
1 C10 GATGCACCCACTGGACTCCT 55
2 C3 CCATTGTTGGCACATTCCGG 55
B) PCR reaction mix
component l
C10 (10 M) 1.0
C3 (10 M) 1.0
10x buffer (750 mM Tris-HCl pH 8.8,
200 mM (NH
4
)
2
SO
4
, 0.1% Tween 20)
2.5
25 mM MgCl
2
1.5
dNTPs (1 mM) 5.0
Betaine (5 M) 3.75
DMSO (10%) 1.25
Platinum Taq (5 units /l) 0.1
DNA template (100 ng/l) 1.0
Water 12.9
C) Gel electrophoresis conditions
Run PCR products of reaction mixture 1 out on 2% (1:1 Nusieve:agarose ) gel for 2
hours, in lane next to those of reaction mixture 2. See Table 5.14 for interpretation of
results.
D) Product sizes
PCR Fragment size (bp) Genotype Product of primers
No product
+
-thalassaemia: -
3.7
1 + 2
1900 Normal () 1 + 2
1900 : (anti 3.7) 1 + 2
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
4.2 PCR protocol for the diagnosis of the (anti 3.7) allele: reaction mix 2
E) Primer sequences
primer Description sequence Annealing temp
0
C
1 C10 GATGCACCCACTGGACTCCT 50
2 C2 CCATGCTGGCACGTTTCTGA 50
F) PCR reaction mix
Component l
C10 (10 M) 1.0
C2 (10 M) 1.0
10x buffer (750 mM Tris-HCl pH 8.8,
200 mM (NH
4
)
2
SO
4
, 0.1% Tween 20)
2.5
25 mM MgCl
2
1.5
dNTPs (1 mM) 5.0
Betaine (5 M) 3.75
DMSO (10%) 1.25
Platinum Taq (5 units /l) 0.1
DNA template (100 ng/l) 1.0
Water 12.9
G) Gel electrophoresis conditions
Run PCR products of reaction mixture 2 out on 2% (1:1 Nusieve:agarose ) gel for 2
hours, in lane next to those of reaction mixture 1. See Table 5.14 for interpretation of
results.
H) Product sizes
PCR Fragment size (bp) Genotype Product of primers
2100 Normal () 1 + 2
2100 : (anti 3.7) 1 + 2
1900
+
-thalassaemia: -
3.7
1 + 2
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
4.3 Interpretation of the results of reaction mixes 1& 2 for the diagnosis of the
(anti 3.7) allele.
A) Products (bp)
Genotypes
Primers: C2+C10
Primers: C3+C10
/ 2100 1900
-
3.7
/ 2100 + 1900 1900
-
3.7
/ -
3.7
1900
/ -
3.7
2100 + 1900 2100 + 1900
/ or / 2100 2100 + 1900
Notes:
i. allele: amplifies with C3+C10 (1.9kb) and C2+C10 (2.1kb).
ii. The -
3.7
allele: amplifies with only C2+C10. Gives a shorter
product (1.9kb) than normal because of the deleted -gene.
iii. The allele: amplifies with C3+C10 (1.9kb) and twice with
C2+C10 (2.1kb) because of the extra -gene.
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Electronic Infrastructure
For Thalassaemia Research Network
B) Possible gel patterns
-genotypes
/ -
3.7
/ -
3.7
/ -
3.7
/ -
3.7
/ or
/
Primer pairs
C2+C10 C3+C10 C2+C10 C3+C10 C2+C10 C3+C10 C2+C10 C3+C10 C2+C10 C3+C0
Band patterns
____
____
____
____
____
____
2.1 kb
____ ____ ____ ____
____ ____ ____
1.9 kb
Figure 5.10.
The diagnosis of
+
-thalassaemia deletion mutations by multiplex GAP PCR using
the primers described in Table 5.9.
H
i
n
d
I
I
I
H
i
n
d
I
I
I
X
1
7
4
X
1
7
4
3
.
7
/
3
.
7
/
3
.
7
3
.
7
/
4
.
2
4
.
2
/
3
.
7
/
4
.
2
4
.
2
/
4
.
2
12
Electronic Infrastructure
For Thalassaemia Research Network
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
Figure 5.11
The diagnosis of
0
-thalassaemia deletion mutations by multiplex GAP PCR using the
primers described in Tables 5.10 & 5.11.
X
1
7
4
X
1
7
4
S
E
A
/
S
E
A
/
S
E
A
T
H
A
I
/
F
I
L
/
M
E
D
/
)
2
0
.
5
/
References
1. Embury, S. H. (1995) Advances in the prenatal and molecular diagnosis of the
haemoglobinopathies and thalassaemias. Hemoglobin 19, 237-261
2. Old, J. (1996) Haemoglobinopathies. Prenat Diag 16, 1181-1186.
3. Old JM. Prenatal Diagnosis of the Haemoglobinopathies. In: Genetic Disorders and the Fetus.
Fourth Edition. Ed. A Milunksy. The Johns Hopkins University Press, Baltimore and London
(1998) p581-612.
4. Old JM. DNA-based diagnosis of hemoglobin disorders. In: Disorders of Hemoglobin. Eds. M. H.
Steinberg, B. G. Forget, D. R. Higgs, R. N. Nagel, Cambridge University Press, Cambridge, UK
(2001), pp.941-957
5. Dode, C., Krishnamoorthy, R., Lamb, J. & Rochette, J. (1992) Rapid analysis of -a
3.7
thalassaemia and aaa
anti 3.7
triplication by enzymatic amplification analysis. British Journal of
Haematology, 82, 105.
6. Bowden, D. K., Vickers, M. A. and Higgs, D. R. (1992) A PCR-based strategy to detect the
common severe determinants of a-thalassaemia. Brit J Haemat 81, 104-108.
7. Baysal, E. and Huisman, T. H. J. (1994) Detection of common deletional a-thalassaemia-2
determinants by PCR. Am J Hematol 46, 208.
8. Liu, Y. T., Old, J. M., Fisher, C. A., Weatherall, D. J. and Clegg, J. B. (1999) Rapid detection of a-
thalassaemia deletions and a-globin gene triplication by multiplex polymerase chain reactions. Brit
J Haemat 108, 295-299.
9. Chong, S. S., Boehm, C. D., Higgs, D. R. and Cutting, G. R. (2000) Single-tube multiplex-PCR
screen for common deletional determinants of a-thalassemia. Blood 95, 360-362.
13
Electronic Infrastructure
For Thalassaemia Research Network
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
10. Old, J. M. (1996) Haemoglobinopathies. Community clues to mutation detection, in Methods in
Molecular Medicine, Molecular Diagnosis of Genetic Diseases (Elles, R. ed), Humana Press Inc.,
Totowa, NJ, pp. 169-183
11. Hartveld, K. L., Heister, A. J. G. A. M., Giordano, P. C., Losekoot, M. and Bernini, L. F. (1996)
Rapid detection of point mutations and polymorphisms of the a-globin genes by DGGE and SSCA.
Human Mutation 7, 114-122.
12. Molchanova, T. P., Pobedimskaya, D. D. and Postnikov, Y. V. (1994) A simplified procedure for
sequencing amplified DNA containing the a-2 or a-1 globin gene. Hemoglobin 18, 251.
13. Ko, T. M., Tseng, L. H., Hsieh, F. J. and Lee, T. Y. (1993) Prenatal diagnosis of Hb H disease due
to compound heterozygosity for South-east Asian deletion and Hb Constant Spring by polymerase
chain reaction. Prenat Diag 13, 143
14. Baysal, E. (1995) The b- and d-thalassemia repository. Hemoglobin 19, 213-236.
15. Ristaldi, M. S., Pirastu, M., Rosatelli, C. and Cao, A. (1989) Prenatal diagnosis of b-thalassaemia
in Mediterranean populations by dot blot analysis with DNA amplification and allele specific
oligonucleotide probes. Prenat Diag 9, 629-638.
16. Sutcharitchan, P., Saiki, R., Fucharoen, S., Winichagoon, P., Erlich, H. and Embury, S. H. (1995)
Reverse dot-blot detection of Thai b-thalassaemia mutations. Brit J Haemat 90, 809.
17. Tan, J. A. M. A., Tay, J. S. H., Lin, L. I., Kham, S. K. Y., Chia, J. N., Chin, T. M., Norkamov, B.
T., Aziz, A. O. B. and Wong, H. B. (1994) The amplification refractory mutation system (ARMS):
a rapid and direct prenatal diagnostic techniques for b-thalassaemia in Singapore. Prenat Diag 14,
1077.
18. Cai, S. P. and Kan, Y. W. (1990) Identification of the multiple b-thalassaemia mutations by
denaturing gradient gel electrophoresis. J Clin Invest 85, 550-553.
19. Losekoot, M., Fodde, R., Harteveld, C. L., Van Heeren, H., Giordano, P. C. and Bernini, L. F.
(1991) Denaturing gradient gel electrophoresis and direct sequencing of PCR amplified genomic
DNA: a rapid and reliable diagnostic approach to b thalassaemia. Brit J Haemat 76, 269-274.
20. Craig, J. E., Barnetson, R. A., Prior, J., Raven, J. L., and Thein, S. L. (1994) Rapid detection of
deletions causing db thalassemia and hereditary persistence of fetal hemoglobin by enzymatic
amplification. Blood 83, 1673-1682.
21. Kafatos F.C., Jones C.W., and Efstratiadis A. Determination of nucleic acid sequence homologies
and relative concentrations by dot blot hybridization procedure. Nucleic Acid Res. 1979, 7:1541-
1552
22. Saiki R.K., Walsh P.S., Levenson C.H., Erlich H.A. Genetic analysis of amplified DNA with
immobilized sequence-specific oligonucleotide probes. Prot. Natl Acad Sci USA. 1989, 86:6230-
6233.
23. Maggio A., Giambona A., Cai S.P., Wall J., Kan Y.W., Chehab C. Rapid and simultaneous typing
of hemoglobin S, hemoglobin C, and seven Mediterranean b-thalassemia mutations by covalent
reverse dot blot analysis: Application to prenatal diagnosis in Sicily. 1993, Blood 81:239- 343.
24. Giambona A., Lo Gioco P., Marino M., Abate I., Di Marzo R., Renda M., Di trapani F., Messana
F., Siciliano S., Rigano P., Cheab F.F., Kazazian H.H., Maggio A. The great heterogeneity of
thalassemia molecular defect in Sicily. Human Genetics 1995, 95: 526-530
25. Foglietta E., Bianco I., Maggio A., Giambona A. Rapid detection of six common Mediterranean
and three non-Mediterranean a-thalassemia point mutations by reverse dot blot. American Journal
of Hematology 2003 November, 74 #3 pg 191-195.
26. Newton, C. R., Graham, A. and Heptinstall, L. E. (1989) Analysis of any point mutation in DNA.
The amplification refractory mutation system (ARMS). Nucl Acids Res 17, 2503-2516.
27. Kwok, S., Kellogg, D. E., McKinney, N., Spasic, D., Goda, L., Levenson, C. and Sninsky, J. J.
(1990) Effects of primer-template mismatches on the polymerase chain reaction: human
immunodeficiency virus type I model studies. Nucl Acids Res 18, 999-1005.
14
Electronic Infrastructure
For Thalassaemia Research Network
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
28. Little S, (1994) Amplification-Refractory Mutation System (ARMS) analysis of point mutations.
In: Current Protocols in Human Molecular Genetics. (Eds. Nicholas C Dracopoli et al.), John
Wiley & Sons, Inc. New York, pp9.8.1. 9.8.12.
29. Antonarakis S.E., Boehm, C.D., Diardina, P.J.V. & Kazazian, H.H.J. (1982) Non-random
association of polymorphic restriction sites in the b-globin gene cluster. Proceedings of the
National Academy of Sciences, USA, 79, 137-141.
30. Chakravarti, A., Buetow, K.H., Antonarakis, S.E., Waber, P.G., Boehm, C.D. & Kazazian, H.H.
(1984) Non-uniform recombination within the human b-globin gene cluster. American Journal of
Human Genetics, 71, 79.
31. Orkin, S.H., Little, P.F.R., Kazazian, H.H., Jr. & Boehm, C.D. (1982) Improved detection of the
sickle mutation by DNA analysis. New England Journal of Medicine, 307, 32-36.
32. Semenza, G.L., Dowling, C.E. & Kazazian, H.H., Jr. (1989) Hinf I polymorphisms 3' to the
human b globin gene detected by the polymerase chain reaction (PCR). Nucleic Acids Research,
17, 2376.
33. Faa, V., Rosatelli, M. C., Sardu, R., Meloni, A., Toffoli, C. and Cao, A. (1992) A simple
electrophoretic procedure for fetal diagnosis of b-thalassaemia due to short deletions. Prenat Diag
12, 903-908.
34. Waye, J. S., Cai, S.-P., Eng, B., Clark, C., Adams III, J. G., Chui, D. H. K. and Steinberg, M. H.
(1991) High haemoglobin A
2
b
o
thalassaemia due to a 532 bp deletion of the 5' b-globin gene
region. Blood 77, 1100-1103.
35. Old, J. M., Varawalla, N. Y. and Weatherall, D. J. (1990) The rapid detection and prenatal
diagnosis of beta thalassaemia in the Asian Indian and Cypriot populations in the UK. Lancet 336,
834-837.
36. Thein, S. L., Hesketh, C., Brown, K. M., Anstey, A. V. and Weatherall, D. J. (1989) Molecular
characterisation of a high A
2
b thalassaemia by direct sequencing of single strand enriched
amplified genomic DNA. Blood 73, 924-930.
37. Dimovski, A. J., Efremove, D. G., Jankovic, L., Plaseska, D., Juricic, D. and Efremov, G. D.
(1993) A b
o
thalassaemia due to a 1605 bp deletion of the 5' b-globin gene region. Brit J Haemat
85, 143-147.
38. Lynch, J. R., Brown, J. M., Best, S., Jennings, M., W. and Weatherall, D. J. (1991)
Characterisation of the breakpoint of a 3.5 kb deletion of the b-globin gene. Genomics 10, 509-
511.
39. Craig, J. E., Kelly, S. J., Barnetson, R. and Thein, S. L. (1992) Molecular characterisation of a
novel 10.3 kb deletion causing b-thalassaemia with unusually high Hb A
2
. Brit J Haemat 82, 735-
744.
40. Waye, J. S., Eng, B., and Hunt, J. A., and Chui, D. H. K. (1994) Filipino b-thalassaemia due to a
large deletion: identification of the deletion endpoints and polymerase chain reaction (PCR)-based
diagnosis. Hum Genet 94, 530-532
41. Decorte, R., Cuppens, H., Marynen, P. & Cassiman, J.-J. (1990) Rapid detection of hypervariable
regions by the polymerase chain reaction technique. DNA Cellular Biology, 9, 461-469.
42. Myers RM, Maniatis T, Lerman LS. Detection and localization of single base changes by
denaturing gradient gel electrophoresis. Methods Enzymol. 155: 501-527, 1987.
43. Sheffield VC, Beck JS, Stone EM, Myers RM. A simple and efficient method for attachment of o
40-base pair, GC-rich seqence to PCR-amplified DNA. BioTecniques, 12: 386-387, 1989.
44. Lerman LS, Silverstein K. Computational simulation of DNA melting and its application to
denaturing gradient gel electrophoresis. Methods Enzymol. 155: 482-501, 1987.
15
Electronic Infrastructure
For Thalassaemia Research Network
h
t
t
p
:
/
/
p
o
r
t
a
l
.
i
t
h
a
n
e
t
.
e
u
45. Losekoot M, Fodde R, Harteveld CL, van Heeren H, Giordano PC, Bernini LF. Denaturing
gradient gel electrophoresis and direct sequencing of PCR amplified genomic DNA: a rapid and
reliable diagnostic approach to beta thalaessemia. Brit J Haematol 76: 274-296, 1990.
46. Ghanem N, Girodon E, Vidaud M, Martin J, Fanen P, Plassa F, Goossens M.A comprehensive
scanning method for rapid detection of beta-globin gene mutations and polymorphisms. Hum
;1:229-239, 1992.
47. Harteveld CL, Heister AJ, Giordano PC, Losekoot M, Bernini LF. Rapid detection of point
mutations and polymorphisms of the -globin genes by DGGE and SSCA. Hum Mutation 7, 114-
122, 1996.
48. Papadakis M, Papapanagiotou E, Loutradi-Anagnostou A. Scanning method to identify the
molecular heterogeneity of delta-globin gene especially in delta-thalassemias: detection of three
novel substitutions in the promoter region of the gene. Hum Mutat 1997;9(5):465-472
49. Keilman MF, Harteveld KL, Bernini LF. Denaturing Gradient Gel Electrophoresis (DGGE) in
Asia-Pacific Course on The Detection of Single-Base mutations: A Laboratory Manual, Eds:
Fucharoen S, Winichagoon P, Kattamis C, Bernini L. 1994.
50. Vrettou C, Palmer G, Kanavakis E, Tzetis M, Antoniadi T, Mastrominas M et al. A widely
applicable strategy for single cell genotyping of -thalassaemia mutations using DGGE analysis:
application to preimplantation genetic diagnosis. Prenatal Diagnosis 1999; 19: 1209-1216.
51. Orkin SH, Kazazian HH, Antonarakis SE, Goff SC, Boehm CD, Sexton JP, Waber PG, Giardina
PJ. 1982. Linkage of -thalassaemia mutations and -globin gene polymorphisms with DNA
polymorphisms in the human -globin gene cluster. Nature 296:627-631.
52. Sanger F, Nicklen S, Carlson AR. DNA sequencing with chain-terminating inhibitors. Proc Natl
Acad Sci 74: 5463-5467, 1977.
53. Wilson RK, Mardis ER. Fluorescence-based DNA sequencing> In Genome Analysis: A
Laboratory Manual. Vol 1 Analysing DNA. (ed Birren B et al, pp301-395, Cold Spring Harbor
Laboratory Press, Cold Spring Harbor, New York, 1997
54. Liu TC, Yen JS, Shan JS, Chen YH, Lee LS, Chen PH & Chang JG. (1992) Rapid molecular
diagnosis of hemoglobin variants. Hemoglobin 16 (5) 379-388
55. Chomczynski P & Sacchi N (1987) Single-step method of RNA isolation by acid guanidinum
thiocyanate-phenol-chloroform extraction. Anal. Biochem. 162, 156-159.
You might also like
- Cell Division Student Exploration SheetDocument5 pagesCell Division Student Exploration SheetKimberly Godoy Mejia100% (2)
- QA in Hematology: Standards, Proficiency, and Quality ControlDocument29 pagesQA in Hematology: Standards, Proficiency, and Quality ControlAmanuel MaruNo ratings yet
- Lipids 1Document56 pagesLipids 1Kim TangoNo ratings yet
- Techtalk August2010Document2 pagesTechtalk August2010Abu KhalidNo ratings yet
- Molecular Diagnosis in HaematologyDocument23 pagesMolecular Diagnosis in HaematologyUmar'Farouq Oni100% (1)
- Quality Lectures - Pre-Analytic Variables - Dr. Tamer SolimanDocument323 pagesQuality Lectures - Pre-Analytic Variables - Dr. Tamer Solimanola bakryNo ratings yet
- How to Dilute Blood and Count White Blood CellsDocument2 pagesHow to Dilute Blood and Count White Blood CellsAlfred ChowNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Nosocomial infections and their preventionDocument48 pagesNosocomial infections and their preventionNovita Trilianty MagdalenaNo ratings yet
- 1111 Chemical Composition of Berry Essential Oils From Juniperus Communis L. From MACEDONIA PDFDocument10 pages1111 Chemical Composition of Berry Essential Oils From Juniperus Communis L. From MACEDONIA PDFGaston CassaroNo ratings yet
- CRISPR HandbookDocument18 pagesCRISPR Handbookgoucloud100% (1)
- Interpretasi Darah RutinDocument22 pagesInterpretasi Darah Rutinboy jendri huluNo ratings yet
- Nephelometry LODocument8 pagesNephelometry LOSantiagoAFNo ratings yet
- Figure 5-6: Virus Infected Body CellDocument10 pagesFigure 5-6: Virus Infected Body CellKaren Flores BartoloNo ratings yet
- Nucleolus and Mitochondria Key OrganellesDocument29 pagesNucleolus and Mitochondria Key OrganellesMicah Lou Calamba100% (2)
- Laboratory Diagnosis of Hypersensitivity and AutoimmunityDocument41 pagesLaboratory Diagnosis of Hypersensitivity and AutoimmunityDenish Calmax AngolNo ratings yet
- Kami Export - Lam Nguyen - Worksheet - Plant Animal CellsDocument2 pagesKami Export - Lam Nguyen - Worksheet - Plant Animal Cellsapi-552399149No ratings yet
- Liver AbscessDocument14 pagesLiver AbscessMariaOeiNo ratings yet
- Sp0005. Platelet Antibody Direct - Pakplus (Elisa)Document7 pagesSp0005. Platelet Antibody Direct - Pakplus (Elisa)yennieyenfulNo ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Slide Preparation of Cerebrospinal Fluid For Cytological ExaminationDocument3 pagesSlide Preparation of Cerebrospinal Fluid For Cytological ExaminationMurshed HaidarNo ratings yet
- Platlets DisorderDocument177 pagesPlatlets DisorderFatimah A Al-dawoodNo ratings yet
- Platelet Counts: Historical Perspectives and Case StudiesDocument35 pagesPlatelet Counts: Historical Perspectives and Case Studiesshikhar623No ratings yet
- Clinical Molecular Diagnostic Techniques: A Brief ReviewDocument19 pagesClinical Molecular Diagnostic Techniques: A Brief ReviewSorin LazarNo ratings yet
- 03 - Approach Hematolymphoid NeoplasmsDocument119 pages03 - Approach Hematolymphoid NeoplasmscandiddreamsNo ratings yet
- Hematology & Oncology #1 Embryology Histology QuizDocument84 pagesHematology & Oncology #1 Embryology Histology QuizSangeeta Yadav100% (1)
- Manual Differential Cell Count LabDocument9 pagesManual Differential Cell Count LabFatima Mae LusanNo ratings yet
- Significance of HbA2 in Screening for HemoglobinopathiesDocument18 pagesSignificance of HbA2 in Screening for HemoglobinopathiesPaula MadureuraNo ratings yet
- Principles, Applications and InterpretationsDocument64 pagesPrinciples, Applications and InterpretationsAbbi Yanto ArtNo ratings yet
- Tumor Markers: Bethy S. Hernowo Dept. of Pathology Anatomy UNPAD/ Hasan Sadikin Hospital BandungDocument31 pagesTumor Markers: Bethy S. Hernowo Dept. of Pathology Anatomy UNPAD/ Hasan Sadikin Hospital BandungDini DesmonaNo ratings yet
- Monoclonal GammopathiesDocument70 pagesMonoclonal GammopathiesElisa Lincă100% (1)
- Clinical Use PT and APTTDocument25 pagesClinical Use PT and APTTMustakim DuharingNo ratings yet
- Immunology in Haematology (Part 2)Document55 pagesImmunology in Haematology (Part 2)kiedd_04100% (4)
- Genome Editing: Toni Cathomen Matthew Hirsch Matthew Porteus EditorsDocument276 pagesGenome Editing: Toni Cathomen Matthew Hirsch Matthew Porteus EditorsSorin Dinu100% (2)
- Formalin Fixative: Making 10% Neutral Buffered Formalin From Stock SolutionsDocument1 pageFormalin Fixative: Making 10% Neutral Buffered Formalin From Stock SolutionsKavisa GhoshNo ratings yet
- Introduction To Parasitology: Pamanatasan NG Lungsod NG Maynila Modified By: Maria Cielo B. Malijan, MD, DPPS, FPSDBPDocument39 pagesIntroduction To Parasitology: Pamanatasan NG Lungsod NG Maynila Modified By: Maria Cielo B. Malijan, MD, DPPS, FPSDBP2013SecBNo ratings yet
- HEMOGLOBINOPATHY GUIDEDocument3 pagesHEMOGLOBINOPATHY GUIDEChatie PipitNo ratings yet
- Clinical Chemistry: Learning Guide SeriesDocument119 pagesClinical Chemistry: Learning Guide Seriesfysi mackNo ratings yet
- Cancer BiomarkersDocument7 pagesCancer Biomarkersmaheen_aslam6596No ratings yet
- Protocol - Gap PCR IthapediaDocument9 pagesProtocol - Gap PCR IthapediaAnh TranNo ratings yet
- Arms ProtocolDocument15 pagesArms ProtocolMahmOod Gh0% (1)
- 2.5 Antibody ScreeningDocument5 pages2.5 Antibody ScreeningBALAJINo ratings yet
- CC1 - Topic 1Document11 pagesCC1 - Topic 1Marie MontemarNo ratings yet
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFDocument16 pagesHarrisADVIA2120methods LabHema2005 11 47-61 PDFedu_14cNo ratings yet
- Department of Pathology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu, IndiaDocument14 pagesDepartment of Pathology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu, IndiaaishaNo ratings yet
- ABO Blood GroupDocument42 pagesABO Blood Groupjong188No ratings yet
- Automated Versus Manual Platelet Count in Aden 2161 0681-3-149Document4 pagesAutomated Versus Manual Platelet Count in Aden 2161 0681-3-149Jeffry MaglalangNo ratings yet
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListPeng KwanNo ratings yet
- Orac MethodDocument5 pagesOrac MethodPriscillaL.SilvaNo ratings yet
- Predanalitika KoagulacijaDocument10 pagesPredanalitika KoagulacijaAnonymous w4qodCJNo ratings yet
- PrinsDocument44 pagesPrinsPalagiri MadhuNo ratings yet
- Alpha Fetoprotein (Afp)Document10 pagesAlpha Fetoprotein (Afp)Andi UkengNo ratings yet
- CE (Ra) F (SH) PF1 (MJ GG) PFA (PR SS)Document4 pagesCE (Ra) F (SH) PF1 (MJ GG) PFA (PR SS)Krishna DubeyNo ratings yet
- Bilirubin Calibrator PDFDocument2 pagesBilirubin Calibrator PDFInsan KamilNo ratings yet
- Applications of PCR in MycologyDocument373 pagesApplications of PCR in Mycologybh1456150% (2)
- Manual and Semiautomatic Hematology TestingDocument10 pagesManual and Semiautomatic Hematology TestingNathaniel Sim100% (1)
- Automated Hematology Cell Counters - ImpedanceDocument14 pagesAutomated Hematology Cell Counters - ImpedanceNoth MT Bnk100% (1)
- Hla B 27 SopDocument12 pagesHla B 27 SopRajeev PareekNo ratings yet
- The Diagnostic Use of ADVIA 2120i Siemens and An "APL Criteria" CanDocument9 pagesThe Diagnostic Use of ADVIA 2120i Siemens and An "APL Criteria" CananggaririnNo ratings yet
- 2016 Jagt 4th QTRDocument48 pages2016 Jagt 4th QTRczumoffenNo ratings yet
- Dry Chemestry HistoryDocument6 pagesDry Chemestry HistoryIdali AuralNo ratings yet
- Cast in Urine SedimentDocument3 pagesCast in Urine Sedimentfirie100% (1)
- Instrumental Analysis in ResearchDocument271 pagesInstrumental Analysis in Researchkb2009No ratings yet
- The Peripheral Blood FilmDocument5 pagesThe Peripheral Blood FilmanggaririnNo ratings yet
- Hematology AnalyzerDocument35 pagesHematology AnalyzerSeemab AhmadNo ratings yet
- Comprehensive Report On Rapid Plasma Reagin Test (RPR)Document3 pagesComprehensive Report On Rapid Plasma Reagin Test (RPR)Kim RuizNo ratings yet
- Impatience Balasamnia 1Document3 pagesImpatience Balasamnia 1vishankguptaNo ratings yet
- Bloodmeal AnalysisDocument2 pagesBloodmeal AnalysisvishankguptaNo ratings yet
- Extraction of DNA From Whole BloodDocument5 pagesExtraction of DNA From Whole BloodvishankguptaNo ratings yet
- DNA Extraction From Fungi, Yeast, and BacteriaDocument2 pagesDNA Extraction From Fungi, Yeast, and Bacteriavishankgupta100% (1)
- Extraction of DNA From Whole BloodDocument5 pagesExtraction of DNA From Whole BloodvishankguptaNo ratings yet
- Glucose IsomeraseDocument5 pagesGlucose IsomerasevishankguptaNo ratings yet
- The Nature of Malathion Resistance in A PopulationDocument4 pagesThe Nature of Malathion Resistance in A PopulationvishankguptaNo ratings yet
- Hepatitis B ElisaDocument5 pagesHepatitis B ElisavishankguptaNo ratings yet
- Introduction 2 Basics of ComputersDocument8 pagesIntroduction 2 Basics of ComputersvishankguptaNo ratings yet
- Periodic TableDocument2 pagesPeriodic TablevishankguptaNo ratings yet
- Genes & Populations: National Institutes of HealthDocument12 pagesGenes & Populations: National Institutes of HealthvishankguptaNo ratings yet
- My Paper On Secondary Fungal Infection in Cancer..Document7 pagesMy Paper On Secondary Fungal Infection in Cancer..vishankguptaNo ratings yet
- Fundamental DutiesDocument2 pagesFundamental DutiesvishankguptaNo ratings yet
- MISCELLANEOUS BLOOD GROUP ANTIGENSDocument4 pagesMISCELLANEOUS BLOOD GROUP ANTIGENSIan Leo SantosNo ratings yet
- KBSM T4 Biologi K1Document24 pagesKBSM T4 Biologi K1Eliza FatimahNo ratings yet
- Struktur Gen, Genom, PolimorfismeDocument30 pagesStruktur Gen, Genom, PolimorfismeIne RahmaNo ratings yet
- Transposable ElementsDocument17 pagesTransposable ElementsNandu RapakaNo ratings yet
- GATE-Syllabus BiotechnologyDocument2 pagesGATE-Syllabus Biotechnologybmaharaj_1No ratings yet
- Molecular Biology - WikipediaDocument9 pagesMolecular Biology - WikipediaLizbethNo ratings yet
- GlycolysisDocument2 pagesGlycolysisapi-323720899No ratings yet
- Test Bank For Human Physiology 14th EditionDocument50 pagesTest Bank For Human Physiology 14th Editionsamanthadayphdamdzkyirej100% (25)
- Sarcopenia, Frailty and Their Prevention by ExerciseDocument22 pagesSarcopenia, Frailty and Their Prevention by ExerciseJoe PolancoNo ratings yet
- Medical Physiology - Principles For Clinical MedicineDocument1 pageMedical Physiology - Principles For Clinical MedicineHaitham WahidNo ratings yet
- Remodelled Biotech Curriculum - Medical Biotechnology 2Document54 pagesRemodelled Biotech Curriculum - Medical Biotechnology 2RishiNo ratings yet
- Test Bank For Microbiology With Diseases Taxonomy 4th Edition BaumanDocument26 pagesTest Bank For Microbiology With Diseases Taxonomy 4th Edition Baumana790342823No ratings yet
- MICROORGANISM SELECTION FOR BIOTECHNOLOGY INDUSTRYDocument21 pagesMICROORGANISM SELECTION FOR BIOTECHNOLOGY INDUSTRYDina Rahma FadlilahNo ratings yet
- Acc Makalah Semhas AltalarikDocument10 pagesAcc Makalah Semhas AltalarikIgede Arya WedaNo ratings yet
- Covid-19 RT PCR Test: Ms. Pranali Kakad Age/SexDocument1 pageCovid-19 RT PCR Test: Ms. Pranali Kakad Age/SexMOHINI ASWARNo ratings yet
- Chap 12Document86 pagesChap 12chemptnkNo ratings yet
- Lecture 2Document32 pagesLecture 2alizeh amanNo ratings yet
- DNA (Deoxyribonucleic Acid)Document5 pagesDNA (Deoxyribonucleic Acid)Sagar MohanNo ratings yet
- SCIENCE 10 (4TH Quarter) - HeredityDocument7 pagesSCIENCE 10 (4TH Quarter) - HeredityJyña Khura TanoNo ratings yet
- Cyclic GMP Synthesis, Metabolism, and FunctionDocument353 pagesCyclic GMP Synthesis, Metabolism, and FunctionpawnammalNo ratings yet
- Insect Pathogens-Molecular Approaches and TechniquesDocument434 pagesInsect Pathogens-Molecular Approaches and Techniquesjulio castilloNo ratings yet
- Angiogenic Growth FactorsDocument9 pagesAngiogenic Growth FactorsArchana Kumari ShawNo ratings yet
- Kocluhetemoglu 2018Document5 pagesKocluhetemoglu 2018adNo ratings yet