Professional Documents
Culture Documents
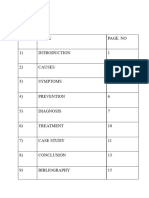
Assessing a Febrile Child for Meningococcal Disease
Uploaded by
Abbas FadelOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessing a Febrile Child for Meningococcal Disease
Uploaded by
Abbas FadelCopyright:
Available Formats
What might sudden onset of illness in an otherwise well child suggest?
Making the diagnosis: Taking the history Meningococcal disease is extremely unpredictable. The presentation can be very varied and patients may be difficult to differentiate from those with viral illnesses during the early stages. Most children with MD present as an acutely febrile child and may not have a rash in the early stages. It is important to take a detailed history and ask parents about the specific symptoms of septicaemia and meningitis. Beware of simply eyeballing a child and assuming they have a trivial illness. This is how many mistakes are made. Make sure you have understood what exactly is worrying the parent and why they are seeking help at this point. Be careful if the child has had contact with a case of meningococcal disease even if they have had prophylactic antibiotics as they can still become ill. Ask about travel to sub-Saharan Africa or contact with Hajj pilgrims. At the initial assessment look for signs and symptoms of septicaemia or meningitis. Some symptoms can be subtle and must be specifically asked about when taking a history
What do you think of this assessment? INITIAL ASSESSMENT OF ANY FEBRILE CHILD For all febrile children the following should be undertaken: Fully undress and examine systematically. Make a thorough search for a focus of infection: think about the hidden sites such as meninges, urinary tract and bloodstream (septicaemia). Mildly pink tympanic membranes or throat do not constitute a focus. If a rash is found, it is important to decide if it is non-blanching. All febrile children with haemorrhagic rashes must be taken very seriously. Although many children with fever and petechiae will have viral illnesses, there is no room for complacency when assessing these children. They must all have their vital signs measured (see below), a decision made as to whether they have signs of meningitis or septicaemia and given intravenous antibiotics. A senior paediatrician should be informed immediately. Children without a rash or with a blanching rash can still have MD. The rash may appear later or not at all if the child has pure meningitis and occasionally with septicaemia. Thorough clinical assessment should ascertain whether there are physical signs of serious systemic illness. The following clinical signs must be measured and recorded to complete a full assessment: -Temperature -Heart rate -Respiratory rate -Blood pressure -Capillary refill time or toe-core temperature gap -Oxygen saturation measurement (normal value is >95% in air) -Assessment of conscious level -Pupil size and reaction -If rash present record if blanching, extent of rash, speed of development
NORMAL VALUES OF VITAL SIGNS Age <1 1-2 2-5 5-12 Over 12 HR/min 110-160 100-150 95-140 80-120 60-100 RR/min 30-40 25-35 25-30 20-25 15-20 Systolic BP 70 -90 80-95 80-100 90-110 100-120
From Advanced Paediatric Life Support - the Practical Approach. Mackway Jones K, Molyneux E, Philips B, Wieteska S, editors. 3rd ed London: BMJ Books; 2001.
What do these signs tell you? How would you interpret the normal blood pressure in the context of other observations? ASSESSMENT OF A FEBRILE CHILD WITH SUSPECTED MENINGOCOCCAL DISEASE If MD is suspected, the purpose of the initial assessment should be to identify whether shock or raised intracranial pressure is present and the severity of the illness. CLINICAL SIGNS OF SEPTICAEMIC SHOCK Septicaemia will lead to shock and multi-organ failure. Shock is a clinical diagnosis. The signs are a result of circulatory failure. The underlying pathophysiology of septicaemia and the capillary leak syndrome leading to these signs. A child in early shock may still be alert and have a normal blood pressure. The early signs of shock include: -Tachycardia -Cool peripheries (CRT>4 seconds) or toe-core temperature gap of >3 degrees ( temp difference between typmanic and dorsum of foot) -Pallor -Decreased urine output (<1ml/kg/hr) -Tachypnoea secondary to acidosis and hypoxia As shock progresses further signs develop: -Metabolic acidosis with base excess worse than 5 -Hypoxia: PaO2 <10kPa in air or saturation < 95% in air
-Increasing tachypnoea, tachycardia and gallop rhythm Late signs of shock include: -Drowsiness or agitation -Hypotension: blood pressure can be normal until the child is very shocked CLINICAL SIGNS OF MENINGITIS When examining a child for signs of meningitis it is crucial to remember that the younger a child the less likely it will be to have neck stiffness or photophobia (especially those <2 years of age). Be guided by the parents as to whether the child is drowsy or behaving inappropriately. Often parents are quick to recognise that the cry of a baby has changed or they are making poor eye contact. Babies with meningitis may have a full or bulging fontanelle reflecting the raised intracranial pressure. They may feel stiff or have jerky movements or they may be very floppy. Fits are common. Drowsiness or decreased conscious level (or fluctuating level) is a very important sign in children of all ages. Teenagers with meningitis often present in an aggressive and combative manner rather than becoming drowsy. Drug and alcohol intoxication may be suspected. Rash: can be present, but more likely to be scanty or petechial than in septicaemia. CLINICAL SIGNS OF RAISED INTRACRANIAL PRESSURE Children with meningitis are at risk of developing RICP . Signs of RICP are: Falling or depressed conscious level Abnormal posturing: decorticate or decerebrate Dilated pupils or unequal pupils Focal neurology Bradycardia and hypertension Abnormal breathing pattern Cushings triad: slow pulse, raised blood pressure and abnormal breathing pattern late sign of RICP Papilloedema is a late sign, its absence does not mean there cannot be any RICP. The diagnosis of raised intracranial pressure is a clinical one: Routine CT scanning is not indicated in patients with meningitis as CT scans are not sensitive in picking up signs of RICP. Lumbar puncture is contraindicated in patients with signs of raised intracranial pressure as coning can be precipitated.
When conscious level is depressed and/or falling, is severity of disease likely to be worse when signs of meningitis are present, or when they are absent?
CLINICAL FEATURES OF SEVERE DISEASE In the majority of patients, one disease process predominates. Patients presenting with mixed disease will also tend, as the disease worsens, to become either profoundly septicaemic or profoundly meningitic. A few will have combined severe septicaemia with shock and severe meningitis with raised intracranial pressure and these need expert management. Patients presenting with septic shock without meningitis carry the worst prognosis. Although a few patients with meningitis will die from raised intracranial pressure, most deaths from MD result from shock and multi-organ failure. Features which predict poor prognosis at the time of presentation include: Presence of shock Absence of meningism Rapidly progressive purpuric rash Low peripheral white blood cell count Thrombocytopenia Markedly deranged coagulation Depressed conscious level Is the very scanty rash a reassuring sign? THE RASH Most patients with meningococcal septicaemia develop a rash - it is one of the clearest and most important signs to recognise. In meningitis it can be scanty, atypical or even absent. It is crucial to remember that the underlying meningitis or septicaemia may be very advanced by the time a rash appears. The rapidly evolving haemorrhagic text book rash may be a very late sign, it may be too late to save the childs life by the time this rash is seen. It is very important to examine children for the signs of meningitis or septicaemia and investigate and treat if necessary based on those findings. Early stages In the early stages the rash may be blanching and macular or maculopapular (sometimes confused with flea bites), but it nearly always develops into a nonblanching red, purple or brownish petechial rash or purpura. Isolated pinprick spots may appear where the rash is mainly maculopapular, so it is important to search the whole body for small petechiae, especially in a febrile child with no focal cause. A rapidly evolving petechial or purpuric rash is a sign of very poor prognosis. Although some of the causes of petechial rashes are self-limiting conditions, many others, including MD are fulminant or life-threatening, and a non-blanching rash should therefore be treated as an emergency. The rash can be more difficult to see on dark skin, but may be visible in paler areas, especially the soles of the feet, palms of the hands, abdomen, or on the conjunctivae or palate. Purpuric areas that look like bruises can be confused with injury or abuse. Extensive purpuric areas often over the feet, legs and hands are usually called purpura fulminans.
You might also like
- TB MeningitisDocument18 pagesTB Meningitisjesa34No ratings yet
- Surrogacy AgreementDocument29 pagesSurrogacy AgreementMacduff RonnieNo ratings yet
- Principles of Pharmocodynamics 2 (Autosaved)Document35 pagesPrinciples of Pharmocodynamics 2 (Autosaved)dv94gw9zd8100% (1)
- Case Study MeningitisDocument20 pagesCase Study MeningitisMitch Love100% (5)
- GP Booklet UK March 2019 For WebsiteDocument12 pagesGP Booklet UK March 2019 For WebsiteJohn SecretNo ratings yet
- NeurosepsisDocument29 pagesNeurosepsisRed DevilNo ratings yet
- Febrile Seizures: Definition and ClassificationDocument3 pagesFebrile Seizures: Definition and ClassificationArmin AbasNo ratings yet
- Neonatal SepsisDocument10 pagesNeonatal SepsisClaudelí GonzalezNo ratings yet
- Meningitis: By-Dr Nimco A. MDDocument31 pagesMeningitis: By-Dr Nimco A. MDgibreilNo ratings yet
- Final Infectious Pe - 1Document49 pagesFinal Infectious Pe - 1Ahmad SobihNo ratings yet
- MeningococcemiaDocument5 pagesMeningococcemiaErhiecka BasaNo ratings yet
- MeningitisDocument28 pagesMeningitisMarcelo Fabian Lopez Santa CruzNo ratings yet
- TEACHING KEY - CASES 11 - 15 (Dec. 7 Session)Document7 pagesTEACHING KEY - CASES 11 - 15 (Dec. 7 Session)Kishwar BasithNo ratings yet
- Pediatric Class NotesDocument14 pagesPediatric Class NotesPrasadNo ratings yet
- Febrile SeizureDocument16 pagesFebrile SeizureRashed Shatnawi100% (1)
- MeningitisDocument23 pagesMeningitisPutri RamadhaniNo ratings yet
- Final Infectious Pe - 1-EditDocument59 pagesFinal Infectious Pe - 1-EditAhmad SobihNo ratings yet
- Description: Kawasaki Disease (Mucocutaneous Lymph Node Syndrome) Is A Form of VasculitisDocument4 pagesDescription: Kawasaki Disease (Mucocutaneous Lymph Node Syndrome) Is A Form of VasculitishamporkNo ratings yet
- 101 FullDocument15 pages101 FullhelinNo ratings yet
- Investigatory Project On MeningitisDocument15 pagesInvestigatory Project On MeningitisMaanya PrithianiNo ratings yet
- CHQ GDL 60010 SepsisDocument11 pagesCHQ GDL 60010 SepsissolidtapeNo ratings yet
- KawasakiDocument3 pagesKawasakikatrina_velasco_1No ratings yet
- Approach To Pediatric Periorbital EdemaDocument10 pagesApproach To Pediatric Periorbital EdemaismailtaaaNo ratings yet
- Meningitidis Consists of The Sudden Onset of Fever, Nausea, Vomiting, HeadacheDocument9 pagesMeningitidis Consists of The Sudden Onset of Fever, Nausea, Vomiting, HeadacheEduardo Romero StéfaniNo ratings yet
- PediatricsDocument38 pagesPediatricskhanNo ratings yet
- Approach To Cyanosis in A NeonateDocument8 pagesApproach To Cyanosis in A NeonateSujeetNo ratings yet
- Clinical Approach To Syncope in ChildrenDocument6 pagesClinical Approach To Syncope in ChildrenJahzeel Gacitúa Becerra100% (1)
- Acute Bacterial MeningitisDocument15 pagesAcute Bacterial MeningitisOana StefanNo ratings yet
- Systemic Lupus Erythematosus in Children and AdolescentsDocument2 pagesSystemic Lupus Erythematosus in Children and Adolescentsarlette aviñaNo ratings yet
- Sickle Cell Disease Is An Inherited Disorder in Which Red Blood CellsDocument5 pagesSickle Cell Disease Is An Inherited Disorder in Which Red Blood Cellsjhonnyboy33No ratings yet
- N. Meningitidis (MENINGOCOCCUS) : Meningococcemia/MeningitisDocument5 pagesN. Meningitidis (MENINGOCOCCUS) : Meningococcemia/MeningitisNestley TiongsonNo ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- Which Is A Really Long Time For A Parent To Count When Their Kid Is Not BreathingDocument6 pagesWhich Is A Really Long Time For A Parent To Count When Their Kid Is Not BreathingYogeshRavalNo ratings yet
- Neurologic Disorders in Children: Pediatric NeurologyDocument59 pagesNeurologic Disorders in Children: Pediatric NeurologyGelsey Gelsinator JianNo ratings yet
- uploaddataa_8060Document23 pagesuploaddataa_8060ronald.brown760No ratings yet
- CNS Bacterial Infections: Pediatric Critical Care Medicine Emory University Children's Healthcare of AtlantaDocument47 pagesCNS Bacterial Infections: Pediatric Critical Care Medicine Emory University Children's Healthcare of AtlantaJanPaulaDelaPenaNo ratings yet
- Meningitis (Physical Exam)Document6 pagesMeningitis (Physical Exam)MohammadAwitNo ratings yet
- Danger Signs in NewbornDocument8 pagesDanger Signs in NewbornPrabhu MagudeeswaranNo ratings yet
- Pediatric Patient ProblemsDocument85 pagesPediatric Patient Problemsgoyabeb59No ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument96 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- Meningitis Clinical PresentationDocument10 pagesMeningitis Clinical PresentationAniwat NillakarnNo ratings yet
- Rubella - Pediatrics - MSD Manual Professional EditionDocument4 pagesRubella - Pediatrics - MSD Manual Professional EditionSadia Shafique100% (1)
- Meningitis Symptoms, Causes, TreatmentDocument6 pagesMeningitis Symptoms, Causes, TreatmentSarika YadavNo ratings yet
- Crux 05Document8 pagesCrux 05Rajkishor YadavNo ratings yet
- Misc in ChildrenDocument23 pagesMisc in ChildrenKushalaniNo ratings yet
- Congenital InfectionDocument15 pagesCongenital Infectionamid sultanNo ratings yet
- Patient Info/doctor/febrile-ConvulsionsDocument6 pagesPatient Info/doctor/febrile-Convulsionsholly theressaNo ratings yet
- Inflammation Brain Spinal Cord: Streptococcus Escherichia Coli Listeria Streptococcus PneumoniaeDocument5 pagesInflammation Brain Spinal Cord: Streptococcus Escherichia Coli Listeria Streptococcus PneumoniaeAndrea QuibrantarNo ratings yet
- Dermatology PastestDocument26 pagesDermatology PastestMateen Shukri100% (1)
- Neonatal SepsisDocument6 pagesNeonatal SepsisSunaina AdhikariNo ratings yet
- Management of Neonatal SeizuresDocument17 pagesManagement of Neonatal SeizuresakankshaNo ratings yet
- Congenital SyphilisDocument6 pagesCongenital SyphilisFrozen Pandora MahayaNo ratings yet
- CNS Bacterial Infections GuideDocument47 pagesCNS Bacterial Infections GuideZEMENAY TRUNEHNo ratings yet
- APSGNDocument3 pagesAPSGNmadimadi11No ratings yet
- BMJ Mcqs+Key To RMBR 14-09-2023Document13 pagesBMJ Mcqs+Key To RMBR 14-09-2023Kiran ShahNo ratings yet
- Pediatric SepsisDocument16 pagesPediatric SepsisOsiithaa CañaszNo ratings yet
- Roseola InfantumDocument1 pageRoseola InfantumnadyaszahraaaaNo ratings yet
- Child With Aseptic Meningitis: Diagnosis and TreatmentDocument4 pagesChild With Aseptic Meningitis: Diagnosis and TreatmentCheng XinvennNo ratings yet
- Child Sepsis SymptomsDocument2 pagesChild Sepsis Symptomssyed askariNo ratings yet
- A Simple Guide to Mucocutaneous Lymph Node Syndrome (Kawasaki Disease), Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Mucocutaneous Lymph Node Syndrome (Kawasaki Disease), Diagnosis, Treatment and Related ConditionsNo ratings yet
- Tuberous Sclerosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandTuberous Sclerosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- About Critical Care NursingDocument7 pagesAbout Critical Care NursingaivynNo ratings yet
- Femoral Fractures in Children: Surgical Treatment. Miguel Marí Beltrán, Manuel Gutierres, Nelson Amorim, Sérgio Silva, JorgeCoutinho, Gilberto CostaDocument5 pagesFemoral Fractures in Children: Surgical Treatment. Miguel Marí Beltrán, Manuel Gutierres, Nelson Amorim, Sérgio Silva, JorgeCoutinho, Gilberto CostaNuno Craveiro LopesNo ratings yet
- Mel Tappans Personal Survival Letter Issue 11 (Tappan)Document24 pagesMel Tappans Personal Survival Letter Issue 11 (Tappan)buckonbeach100% (1)
- EEG ArtifactsDocument18 pagesEEG ArtifactsNazwan Hassa100% (1)
- Assignment On PrionsDocument22 pagesAssignment On PrionsRinta Moon100% (2)
- Massive Haemorrhage: P Donnelly B FergusonDocument18 pagesMassive Haemorrhage: P Donnelly B FergusonRizqiNo ratings yet
- 4926-02 L2 Certificate Qualification Handbook v1 PDFDocument116 pages4926-02 L2 Certificate Qualification Handbook v1 PDFforumuse3bNo ratings yet
- Ifrs Issues Solutions For PharmaDocument109 pagesIfrs Issues Solutions For PharmaSrinivasa Rao100% (1)
- Canadian Standards For Hospital LibrariesDocument4 pagesCanadian Standards For Hospital LibrariesFernando HernandezNo ratings yet
- DylasisDocument3 pagesDylasisyuvi087No ratings yet
- Emotional Trauma ClearingDocument13 pagesEmotional Trauma ClearingEstela ParraNo ratings yet
- Case Study: MYXEDEMATOUS COMADocument5 pagesCase Study: MYXEDEMATOUS COMAjisooNo ratings yet
- ICU HandoverDocument2 pagesICU HandoverMark 'Mark Douglas' DouglasNo ratings yet
- Melanoma Cancer PresentationDocument13 pagesMelanoma Cancer PresentationMerlyn JeejoNo ratings yet
- Symposiumbooklet CareerDocument36 pagesSymposiumbooklet Careerroh009No ratings yet
- SextafectaDocument2 pagesSextafectaAndres Felipe Perez SanchezNo ratings yet
- Concrete MSDS 1 PDFDocument5 pagesConcrete MSDS 1 PDFmanil_5100% (1)
- Embryology GenitalDocument53 pagesEmbryology GenitalDhonat Flash100% (1)
- BarryKuebler Lesson1 AssignmentDocument4 pagesBarryKuebler Lesson1 AssignmentBarry KueblerNo ratings yet
- Cerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluidDocument5 pagesCerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluiderickNo ratings yet
- 515Document972 pages515solecitodelmarazul100% (6)
- 1413272524world10 15 14 PDFDocument38 pages1413272524world10 15 14 PDFCoolerAdsNo ratings yet
- Mental Health Personal Statement - Docx'Document2 pagesMental Health Personal Statement - Docx'delson2206No ratings yet
- Drug-Induced Taste Disorders: A Primer for ToxicologistsDocument10 pagesDrug-Induced Taste Disorders: A Primer for ToxicologistsBharat NarumanchiNo ratings yet
- 837 Institutional 5010 PDFDocument610 pages837 Institutional 5010 PDFtrkreddyNo ratings yet
- HEX Character Generation Cheat Sheet Version 3Document20 pagesHEX Character Generation Cheat Sheet Version 3NestorDRod100% (1)
- Fundamentals of Tooth Preparation Periodontal AspectsDocument74 pagesFundamentals of Tooth Preparation Periodontal AspectsVica Vitu100% (3)
- JC Oncology55211005Document32 pagesJC Oncology55211005Neenuch ManeenuchNo ratings yet