Professional Documents
Culture Documents
Health Insurance - Managed Care
Uploaded by
Breanne McBrideOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Health Insurance - Managed Care
Uploaded by
Breanne McBrideCopyright:
Available Formats
Health Care Reform Team E Keller Graduate School of Management June 7, 2010
Health Care Reform and Consumers
Health care reform constitutes the process by which the social policies that regulate health care are created and or modified. In essence, health care reform is driven, to a large extent, by regulatory reform, consumers, and practitioners. Where Health care reform, represents a subset of health care policies, it is important to recognize non-regulatory drivers of health care reform such as the impact of market forces on the level of quality of care, as with the Leapfrog group, and the recent report from the Institute of Medicine regarding medical errors (Schuster, 2008). Health care reform can lead to changes in the degree to which the government controls and manages access of the population to health care and the way in which health care is financed (Mechanic, 2006). Many have passed opinions regarding the role and responsibility of the government in providing health care services, and the underwriting of such services, such as those can be seen in the United States and Canada, do not preclude health care reform from having a profound impact on patients, the public, providers, and payers of these very different systems. Health care reform and oversights has led to diminished independence of the medical profession. This, in turn, has resulted in the current system by which health care providers
are reimbursed for the services and resources that they provide. At one time, the medical profession controlled entry into the health care system and set the prices that would be charged for the delivery of their services (Geyman, 2006). The medical profession determined which hospital a patient would be admitted to, which laboratory a patient would utilize, and where a patient would go for other radiological and ancillary services. Pricing was led by the costs incurred by the provider. To determine pricing, the provider determined its costs and the desired profit margin. Regulation of health care, at that time, was focused on the licensing and accreditation of health care providers (Guglielmo, 2007). In addition, the medical profession determined which hospital a patient would be admitted to, which laboratory a patient would utilize, and where a patient would go for other radiological and ancillary services. Pricing was led by the costs incurred by the provider. To determine pricing, the provider determined its costs and the desired profit margin. Regulation of health care, at that time, was focused on the licensing and accreditation of health care providers (Guglielmo, 2007) However, in the 1970s, because of economic recession and inflation, health care reform became focused on health care cost containment. Primacy was given to the development of
reimbursement policies that would influence the behavior of providers, utilization of health care services, and the attendant medical costs, would be reduced. It is believed no matter what happens with health care reform inequities in the delivery of health care will persist. Some argue that a major problem overlooked by most reform efforts is the chronic undersupply of minority and female physicians. Regardless of good intentions, a health care delivery system reliant upon physicians who are, by and large, white, upper-class, able-bodied, and heterosexual males will inevitably yield poorer health care outcomes for patients who fall outside these categories. Others argue that even if a ready supply of physicians outside these privileged groups existed, inequities sustained by the existing system of medical beliefs remain unaddressed. These barriers stem from the nature of medical training and the ways in which medical knowledge is applied within health care delivery (Mechanic, 2006). Medical professionals are trained to complete the process of diagnosis and treatment by taking symptoms presented by a patient and using make a diagnosis for which they can then prescribe treatment. Patients who receive the best care are those who can most skillfully cooperate in the construction of these standardized medical narratives. Patients who are unfamiliar with the appropriate medical terms and phrases, whose
cases are complicated, or who attempt to present alternative narratives to the standard medical ones are less likely to receive good care (Geyman, 2006). It is believed adding 30 million people into the health care system will translate into a great amount of economic activity and opportunity for millions of Americans: jobs for many doctors, nurses, technicians, administrators and new jobs in research, information technology, and medicine -- not to mention the positive impact it will have on supporting industries and professions. Adding ten percent of the entire US population into a system of continuous preventive care will undoubtedly lead to job and infrastructure growth in an industry that l embodies the best way to improve the general welfare of our nations families. Therefore, a trillion dollar ten-year health care reform package serves double purpose -- not only does it begin to take the steps necessary to provide accessible and affordable health care for everyone, but it also acts as a massive jobs program and stimulus to uplift an economy struggling to recover (Health-care bill). Although Health Care Reform has its disadvantages and advantages it is still viewed as the process by which social
policies that regulate health care are create and driven by regulatory reform of the federal government.
Health Care Reform and the Health Insurance Industry
The health insurance industry will face intense regulatory scrutiny due to the new Patient Protection and Affordable Care Act and its companion, the Health Care and Education Reconciliation Act of 2010. PPACA would create a new system of
health insurance exchanges that would help individuals and small businesses buy subsidized, standardized packages of health benefits. The new exchanges will change the level competition, the researchers say. The effects will be different in each state, and they may include reduction of distribution costs and potentially tempering of rate increases in the individual and small group insurance markets, the researchers add. While new regulation does not necessarily go into effect immediately, it is clear those health insurers now face increased scrutiny and a new layer of regulatory complexity, researchers at Milliman, write in an analysis of the new laws. Health plans will have to focus on minimum loss ratios and administrative efficiency and will have to balance challenging cost dynamics against the need for affordable policies.
Patient Protection and Affordable Care Act of 2010 (PPACA) has left many insurance questions stumbling around for answers and clarification from the federal government. For example, at
Health Care Service Corporation (HCSC) work is under way to help their clients take advantage of PPACAs Early Retiree Reinsurance Program, in which groups that offer coverage to pre65 retirees can be reimbursed by the government for some claims. This program goes into effect for claims starting June 1, 2010, although the employer application will not be available from the government until late June. Several of HCSC employer groups are very interested in applying for this reimbursement; HCSC is left explaining this delay to their accounts as they will be assisting them with claims reporting and other services. Another discrepancy for PPACA is the new minimal Medical Loss Ratio (MLR) rule. This guideline will require that,
starting Jan. 1, 2011, insurers spend at least 85% of large group premium revenue and 80% of small group and individual policy premium revenue on medical care and health care quality improvement activities. Health insurers have many questions regarding the MLR rule. Questions such as, what does the
government consider as medical care and health care quality improvement activities? offer many guidelines. This provision is vague and doesnt
PPACA also refers to grandfathered plans which is a health plan in existence on the date PPACA became law, March 23, 2010. Grandfathered plans are subject to some, but not all, of PPACA's reforms. The reforms that apply to grandfathered plans include restrictions on pre-existing condition limitations, restrictions on lifetime and annual limits, expansion of coverage for adult dependent children, and waiting period restrictions. A number of PPACA's requirements will not apply However, no one knows yet whether, and
to grandfathered plans.
to what extent, a grandfathered plan will retain its grandfathered status once the employer makes material changes to that plan (other than changes to comply with mandatory PPACA requirements.) Accordingly, until more guidance on the grandfather rules becomes available, insurers and employers will want to tread carefully in making material changes to grandfathered plans.
References Mechanic, D. (2006). The Truth about Health Care: Why Reform Is Not Working in America: New Brunswick, NJ: Rutgers University Press: 145-189
Schuster, A. (2008). How Good Is the Quality of Health Care in the United States: The Milbank Quarterly: 76(4): p517563
Geyman, P. (2006). Myths as Barriers to Health Care Reform in the United States: International Journal of Health Services: 33(2):
Guglielmo, W. (2007). Managed care reform? Surebut don't look to Washington: Medical Economics: 23(6): p4041p315329.
http://www.nytimes.com/2010/03/22/business/22bizhealth.htm New York Times. Health Care overhauls Booms Hospital. Retrieved 5-9-2010
Retrieved from: http://www.examiner.com/x-24957-Progressive-Examiner~y2009m12d25-Healthcare-bill-willstimulate-economy-and-create-tens-of-thousands-of-jobs Health-care bill will stimulate economy and create tens of thousands of jobs
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Unit 10 - Insurance - S PDFDocument15 pagesUnit 10 - Insurance - S PDFSofiaNo ratings yet
- IRM MergedDocument71 pagesIRM MergedDhanashree BangarNo ratings yet
- Principles of Risk Management and Insurance 11th Edition Rejda Test BankDocument10 pagesPrinciples of Risk Management and Insurance 11th Edition Rejda Test Bankhelenglendacduf100% (22)
- Manual Martillo Demoledor MakitaDocument24 pagesManual Martillo Demoledor MakitaEdi Obrayan100% (1)
- 8.insurance Law BL1Document6 pages8.insurance Law BL1natsu lolNo ratings yet
- For In-Home Supportive Services Workers: PASC-SEIU Homecare Workers Health Care PlanDocument9 pagesFor In-Home Supportive Services Workers: PASC-SEIU Homecare Workers Health Care PlanMustaffah KabelyyonNo ratings yet
- Math For Business and Finance An Algebraic Approach 1st Edition Slater Solutions ManualDocument6 pagesMath For Business and Finance An Algebraic Approach 1st Edition Slater Solutions Manualxeniaanselmnxcbea100% (25)
- 2012 Standards ManualDocument72 pages2012 Standards ManualSherif Abou BakrNo ratings yet
- Revenue CycleDocument0 pagesRevenue Cyclecasti134No ratings yet
- 15 Things Homeowners Insurance Doesn't Cover: Property Coverage ExclusionsDocument3 pages15 Things Homeowners Insurance Doesn't Cover: Property Coverage ExclusionsAva HayekNo ratings yet
- 2023 Open Enrollment Benefit Presenation - 11142022Document30 pages2023 Open Enrollment Benefit Presenation - 11142022margreen5No ratings yet
- September 2014 MailerDocument35 pagesSeptember 2014 MailerBritCitsNo ratings yet
- Philippine Health Insurance Corporation: Republic of The PhilippinesDocument2 pagesPhilippine Health Insurance Corporation: Republic of The Philippinesangga2681No ratings yet
- Project Report: Pharmacy: CS 6360.002 - TEAM 23Document27 pagesProject Report: Pharmacy: CS 6360.002 - TEAM 23xyzNo ratings yet
- Notice: Medicare: Emergency Medical Treatment and Labor Act Technical Advisory GroupDocument2 pagesNotice: Medicare: Emergency Medical Treatment and Labor Act Technical Advisory GroupJustia.comNo ratings yet
- MVP Silver Summary of Benefits and CoverageDocument6 pagesMVP Silver Summary of Benefits and Coverageksenos.ukNo ratings yet
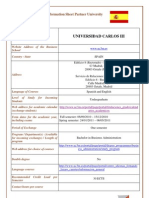
- Carlos IIIDocument5 pagesCarlos IIIqlq1No ratings yet
- Ahip Module 2 (Solved%)Document2 pagesAhip Module 2 (Solved%)WizzardNo ratings yet
- Eligibility Results NoticeDocument12 pagesEligibility Results NoticeLagannNo ratings yet
- Full Life InsuranceDocument7 pagesFull Life InsuranceNisa BhuttaNo ratings yet
- Notice: GR Modifier UseDocument2 pagesNotice: GR Modifier UseJustia.comNo ratings yet
- Accounting Neri & LoiDocument120 pagesAccounting Neri & Loinerissa lopeNo ratings yet
- BankingDocument14 pagesBankingHeral SataNo ratings yet
- Thesis Statement For Life InsuranceDocument8 pagesThesis Statement For Life Insurancednnsgccc100% (2)
- Ayushman BharatDocument3 pagesAyushman BharatSimran SpalNo ratings yet
- MPHP Book ActiveDocument185 pagesMPHP Book ActivetvmixerNo ratings yet
- My Healthcare Is Killing MeDocument142 pagesMy Healthcare Is Killing Mechangehealthcare100% (7)
- Updated NDP ReviewerDocument5 pagesUpdated NDP ReviewerKneth Rye100% (1)
- Loss RatioDocument3 pagesLoss RatiohieutlbkreportNo ratings yet
- Tale of Piracy Unfolds On Facebook: Farewell To Panamah Peat'Document52 pagesTale of Piracy Unfolds On Facebook: Farewell To Panamah Peat'Tad WoottonNo ratings yet