Professional Documents
Culture Documents
Outbreak Guideline
Uploaded by
anonymousOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Outbreak Guideline
Uploaded by
anonymousCopyright:
Available Formats
Document Number # 6
Guideline for the Management of Outbreaks of Communicable Disease in Health Facilities
Custodian/Review Officer: Centre for Healthcare Related Infection Surveillance and Prevention (CHRISP)
1.
Purpose
This Guideline provides recommendations regarding best practice for managing outbreaks of communicable disease (whether notifiable or not) in Queensland Health facilities.
Version no: 2
Applicable To: All Queensland Health facilities
2.
Scope
Approval Date: 19/03/12
Effective Date: 19/03/2012
This Guideline provides information for all Queensland Health employees (permanent, temporary and casual) and all organisations and individuals acting as its agents (including Visiting Medical Officers and other partners, contractors, consultants and volunteers).
Next Review Date: 19/03/2014
Authority:
3.
Related documents
Policy and Standard/s:
Approving Officer Name Dolly Olesen, Director - CHRISP
Queensland Health Prevention and Control of Healthcare Associated Infection (HAI) Policy Queensland Health Prevention and Control of Healthcare Associated Infection (HAI) Standard Duties of Chairperson Outbreak Control Team (OCT) Attachment 1 Outbreak Log Attachment 2 Checklist for Outbreak Control Team (OCT) tasks Attachment 3 Dealing with the Media Attachment 4 Communicable Attachment 5 Diseases of Importance
Supersedes: Queensland Health Guideline for the Management of Outbreaks of Communicable Disease in Health Facilities (2009)
Forms and templates:
Key Words: Outbreak management, communicable disease, Outbreak Control Team, Outbreak Plan
Accreditation References: ACHS EQuIP Standard 1.5.2 SA (e) Australian Commission on Safety and Quality in Health Care, National Safety and Quality Health Service Standard Preventing and Controlling Healthcare Associated Infections
Outbreak Management Checklist Attachment 6.
Version No.: 2
; Effective From: 19/03/2012
Page 1 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
4.
Guideline for Outbreak Management
4.1 Objective of Outbreak Management The objective of outbreak management of communicable diseases is to interrupt transmission as quickly as possible and thus prevent further cases. To accomplish this, it is necessary to: recognise a potential or actual outbreak eliminate the source stop further spread prevent recurrence ensure satisfactory communication between all concerned disseminate lessons learnt.
4.2 Outbreak Control Plan It is recommended that each health facility should have in place a facility-specific Outbreak Control Plan (OCP) that has been developed in consultation with key stakeholders. The OCP is intended to ensure prompt action to recognise an outbreak of communicable disease, eliminate the source and stop further spread, prevent recurrence, and ensure satisfactory communication between all concerned. The OCP should be reviewed periodically but at least every three years. The OCP may include and identify the following: a description of the roles and extent of the responsibilities and accountabilities of each of the organisations and individuals an up-to-date list of stakeholder contact details arrangements for informing and consulting those who need to be aware of an outbreak situation arrangements for creating an outbreak control team to investigate and control a major disease outbreak, the support which will be available to the group and what its duties are the resources required to manage an outbreak staff issues (for example, arrangements for staff to work outside normal working hours) training for all staff involved in investigating communicable disease outbreaks ensuring staff are familiar with requirements for completing and disseminating the final outbreak report.
Version No.: 2; Effective From: 19/03/2012
Page 2 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
4.3 Outbreak Control Team An Outbreak Control Team (OCT) is a multi-disciplinary group which will work together to investigate an outbreak. The core team is responsible for planning and coordinating the investigation. The decision to convene an OCT will be made by relevant personnel, such as the Chairperson of the Infection Control Committee or an Infectious Diseases Physician/Microbiologist. The following factors should be considered in the decision to convene an OCT: the number of cases and the nature of the population at risk the organism/agent and its severity the extent of the outbreak o the number of confirmed or suspected cases (outbreak definition) o large numbers of cases o two or more cases of a notifiable condition in the same ward/area, within the incubation period the likely source the location of the outbreak potential impact on service delivery o involvement of management/Executive is required to implement measures to control disease spread (for example, closure of wards or beds) o involvement of more than one ward or department public concern media interest the potential public health risk.
4.3.1 Outbreak Control Team Membership The coordinator of the OCT will usually be the Infection Control Committee Chairperson or other appropriately qualified person. Refer to Attachment 1 Duties of the Chairperson Outbreak Control Team (OCT) for the roles and responsibilities of the OCT Chairperson. The composition of the OCT may include the following professionals as required: Health Service District Executive member or delegate Chairperson Infection Practitioner/Coordinator Control Committee and/or Infection Control
manager/clinician representatives from the relevant area
Version No.: 2; Effective From: 19/03/2012
Page 3 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
Infectious Diseases Physician and/or Microbiologist (the Chairperson may choose to contact the CHRISP Expert Advisory Group [CEAG] for consultation ph 3328 9755) Population Health Unit representation, when appropriate (e.g. notifiable disease) Media Relations Officer other relevant stakeholders e.g. Occupational Health and Safety, Support Services, Food Services, Sterilizing Services, Pharmacy etc other individuals, including representative of other agencies involved in the outbreak may be co-opted as necessary.
4.3.2 Outbreak Control Team Terms of Reference A central outbreak log (refer to Attachment 2 Outbreak Log for an example) should be kept of all activities associated with the outbreak investigation, including minutes of meetings, delegated tasks and actions taken by team members, laboratory results and other relevant information. Terms of reference for the OCT may include the following: review the evidence and confirm or refute existence of an outbreak; decide whether further investigation is required o to confirm the outbreak, immediate steps must be taken by the facilitys Infection Control Team/Coordinator to collect further clinical, epidemiological and laboratory information. A case definition will be established and used to verify known cases and to search for further possible cases develop a strategy to investigate and control the outbreak allocate tasks to outbreak team members investigate the outbreak and identify the nature, vehicle and source of infection implement control measures and monitor their effectiveness in dealing with the cause of the outbreak including preventing further spread prevent further cases elsewhere by communicating findings to the Communicable Diseases Branch, Queensland Health, where appropriate conduct formal outbreak control meetings on a regular basis document minutes of each OCT meeting including allocated tasks and any actions taken or completed ensure adequate staff and resources are available for the management of the outbreak consider potential staff training opportunities of the outbreak identify and utilise any opportunities for the acquisition of new knowledge about disease control
Version No.: 2; Effective From: 19/03/2012
Page 4 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
provide support, advice and guidance to all individuals and organisations directly involved in dealing with the outbreak, which may include general community, hospital patients, visitors, relatives and staff keep relevant outside agencies, the general public and media appropriately informed declare the conclusion of the outbreak and to prepare a final report evaluate the response to the outbreak and implement changes in OCT procedures based upon lessons learnt.
4.3.3 Outbreak Control Team Procedure The responsibility for making a decision to convene an OCT will depend on the circumstances of the cases and the environment in which the outbreak occurs. Decisions regarding health facility outbreaks ultimately lie with the relevant Health Service District Executive. Therefore, facility specific outbreak management plans shall be developed. In reality, the practical responsibility for such plans usually rests with the Infection Control Team/Coordinator. The following steps outline the general procedure for an OCT. Chairperson to convene OCT elect Secretariat 1. minutes to be taken of all OCT meetings and subsequently approved. These will record details of all issues discussed and decisions made at first OCT meeting: 1. agree on the OCT composition and terms of reference 2. confirm individual responsibilities (refer Attachment 3 Checklist for Outbreak Control Team (OCT) tasks) 3. review checklist of OCT tasks (Attachment 3 Checklist for Outbreak Control Team (OCT) tasks) at each subsequent OCT meeting, the situation should be systematically reviewed and the need to obtain further assistance should be formally considered at the final OCT meeting (determined by Chairperson): 1. review the experience of all involved in management of the outbreak 2. identify any problems encountered 3. prepare the final report (refer to section 4.3.4 Outbreak Control team Communication and Reports for suggested inclusions for the final report) 4. recommend any necessary revisions to the facility-specific outbreak management plan.
Version No.: 2; Effective From: 19/03/2012
Page 5 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
4.3.4 Outbreak Control Team Communication and Reports Communication with relevant stakeholders is a key element of outbreak management. It is the responsibility of the Chairperson of the OCT to determine when to communicate the existence of an outbreak with the local Population Health Unit. Under the Public Health Act 2005 and Public Health Regulation 2005, laboratories notify the chief executive or delegate (public health medical officers are delegated for this purpose) all laboratory-confirmed notifiable conditions. Similarly medical officers and directors of hospitals are required to notify the chief executive or delegate of clinical and provisional diagnosis of notifiable conditions. A complete list is available from: http://www.health.qld.gov.au/ph/documents/cdb/notif_conditions_rpt.pdf. When an OCT is convened, the Chairperson will inform the: Health Service District Executive Infection Control Team/Coordinator relevant facility-based managers/clinicians relevant Population Health Unit (if appropriate) o the local Population Health Unit shall be informed where the outbreak involves a notifiable disease or where the impact of the outbreak gives rise to a broader public interest e.g. where members of the public are recalled for look back investigations or where there is a risk the outbreak may extend to the broader community Senior Director, Communicable Diseases Branch (if appropriate) o some discretion by the facility or Population Health Unit has been factored into the plan by placing responsibility on the Chairperson of the OCT to determine when to communicate the existence of an outbreak with the Division of the Chief Health Officer via the Communicable Diseases Branch o in the first instance, it is a requirement that the local Population Health Unit be informed, however the Senior Director, Communicable Diseases Branch shall be informed where the outbreak involves the following: notifiable disease where the impact of the outbreak gives rise to a broader public interest e.g. members of the public are recalled for look back investigations the primary cause of death of a case is the communicable disease involved in the outbreak
o where the Senior Director is not available, the Senior Medical Officer or the Manager, Communicable Disease Prevention and Control, Communicable Diseases Branch, should be notified. These staff members, once notified will collaborate and have the responsibility of informing other key personnel in the Division of the Chief Health Officer, as appropriate o contact details:
Version No.: 2; Effective From: 19/03/2012
Page 6 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
Senior Director, Communicable Diseases Branch (ph 3328 9723; fax 3328 9782) Senior Medical Officer, Communicable Diseases Branch (ph 3328 9725; fax 3328 9782) Director, Communicable Disease Prevention and Control Unit, Communicable Diseases Branch (ph 3328 9741; fax 3328 9782)
CHRISP (if appropriate) o facilities will correspond with CHRISP regarding outbreaks where further assistance, advice or support is required. This is particularly important where there are state-wide implications particularly in the areas of infection control and sterilizing
the general community (if appropriate) usually via a Media Relations Officer.
During the outbreak, key individuals will be kept informed in accordance with the responsibilities outlined in Attachment 3 Checklist for Outbreak Control Team (OCT) tasks. The OCT should endeavour to keep the public and media as fully informed as possible without prejudicing the investigation and without compromising any statutory responsibilities and legal requirements. Media statements and enquires will be dealt with in accordance with the principles outlined in Attachment 4 Dealing with the Media. At the conclusion of the outbreak, a final report will be prepared by the Chairperson on behalf of the OCT. The final report should be considered a public document and due regard therefore given to confidential aspects of the outbreak investigation. The final report will highlight: the results of the outbreak investigation and control interventions any difficulties or problems encountered any action required to prevent recurrence any recommended revisions to the facility-specific outbreak management plan. health facility: all OCT members, Health Service District Executive, other facilitybased managers/clinicians as appropriate Population Health Unit and CHRISP (where appropriate).
The final report should be circulated as follows:
4.4 The Investigation and Control of an Outbreak Outbreak management tends to fall into four distinct phases. In practice there is considerable overlap between the phases especially between the detection, investigative and response phases. The four phases are described as: outbreak detection outbreak investigation outbreak response
Version No.: 2; Effective From: 19/03/2012 Page 7 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
evaluation of response.
An outbreak is generally defined as occurring whenever disease levels exceed that expected in a given community/population over a specific timeframe. Attachment 5 Communicable Diseases of Importance provides information regarding notifiable diseases and potential communicable diseases which may cause outbreaks. A central outbreak log (refer to Attachment 2 for an example of an Outbreak Log) should be kept of all activities associated with the outbreak, including minutes of meetings, delegated tasks and actions taken by team members, laboratory results and other relevant information. Outbreaks of healthcare associated infections are generally the responsibility of that facilitys Infection Control Committee. However, outbreaks of notifiable diseases may require the involvement of the Population Health Unit. An Outbreak Management Checklist (Attachment 6) may be utilised to guide facilities in the management of outbreaks. 4.4.1 Outbreak Detection Outbreak management begins with the timely identification of an outbreak. Please refer to Section 4.4 The Investigation and Control of an Outbreak for an outbreak definition. Basic steps to help identify if an outbreak exists includes: assessing what is happening e.g. symptoms observed determining the timeline since symptoms first observed / notified define the area where it is happening determining the likely transmission environmental, food or other factors) routes (e.g. human, animal, vector,
determine characteristics of individuals affected (e.g. age, sex, health status).
If an outbreak is confirmed, an initial assessment of the extent and importance of the outbreak will be made and a decision taken on whether to institute the facility-specific outbreak plan and convene the OCT. 4.4.2 Outbreak Investigation Investigation of disease outbreaks involves a combination of epidemiological, laboratory and environmental investigation. A case definition should be established at this point of outbreak management. A case definition is formed by using a standard set of criteria to decide whether, in this investigation, an individual should be classified as having the disease or health condition under study. A case definition usually includes four components: 1. clinical information about the disease 2. characteristics about the people who are affected
Version No.: 2; Effective From: 19/03/2012
Page 8 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
3. information regarding the location or place 4. specification of time during which the outbreak occurred. Once a case definition has been established, attempts should be made to identify additional persons who meet the case definition. This enables a more accurate estimate of the magnitude of the outbreak, it reduces the likelihood of bias which may occur by only focusing on cases detected early in the investigation and it increases the sample size. A structured questionnaire should be used to collect detailed information regarding cases. Information to be collected from each case includes: identifying information demographic information clinical information (date/time of onset, signs and symptoms, hospitalisation, death etc) laboratory information risk factor information (contact with known case, environmental exposures etc) contact with individuals with similar symptoms.
4.4.3 Outbreak Response An outbreak response is characterised by hypothesis-forming and the implementation of relevant control measures. It is important that an OCT is formed in this phase. Please refer to Section 4.3 Outbreak Control Team and Attachment 3 Checklist for Outbreak Control Team (OCT) Tasks for information regarding this important process. The primary goal of outbreak response is control and prevention. Control measures should be considered at all stages of the investigation and implemented as soon as possible. Control measures may be directed at: 1. controlling the source for example, by destroying contaminated foods 2. controlling the spread for example, isolation of cases or contacts, screening and monitoring of contacts, protection of contacts by immunisation or chemo-prophylaxis, closure of beds/wards.
Cooperation and prompt exchange of information is essential to the successful management of communicable disease outbreaks. Effective communication must occur on a number of levels. This may include between health professionals, local government as well as with the wider community. Please refer to Section 4.3.4 Outbreak Control Team Communication and Reports for further communication strategies. 4.4.4 Evaluation of Outbreak Response A thorough evaluation of the outbreak response helps bring about continuous improvements in practice. The aim of the evaluation is to determine if the incident
Version No.: 2; Effective From: 19/03/2012
Page 9 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
objectives were met and to identify positive outcomes and document areas for improvement. The following is a list of criteria that helps guide the evaluation: preparedness for this type of investigation (includes resources, guidelines, questionnaires, databases, etc) coordination of outbreak meetings, communication (including media management) organisation record keeping (responsibility) epidemiology investigation processes and control initiatives implemented.
5.
Definition of Terms
Definitions of key terms are provided below.
Term Case definition Definition / Explanation / Details Is a standard set of criteria to be used in outbreak investigation to decide who is a case and who is not. A case definition should include well-defined clinical symptoms (+/laboratory criteria) and restrictions by time, place and person. Is generally defined as occurring whenever disease levels exceed that expected in a given community/population over a specific timeframe. based Extra work practices in situations where standard precautions alone may be insufficient to prevent infection (e.g. for patients known or suspected to be infected or colonised with infectious agents that may not be contained with standard precautions alone). Source Queensland Health Foodborne Illness Outbreak Management Guidelines 2006
Outbreak
Transmission precautions
Module 9 Outbreak Management: Participant Workbook, Public Health Nurse Communicable Disease Training Program. National Health and Medical Research Council (2010) Australian Guidelines for the Prevention and Control of Infection In Healthcare http://www.nhmrc.gov.au/_files_n hmrc/file/publications/synopses/C D33_InfectionControlGuidelines2 010.pdf. Access date 29/09/2011
6.
References and Suggested Reading
Centres for Disease Control and Prevention. Steps of an Outbreak Investigation. 2004. http://www.cdc.gov/excite/classroom/outbreak/steps.htm Communicable Disease Factsheet. Measles. 2008. http://www.health.gov.au/internet/main/publishing.nsf/Content/cdna-songs-measlesfacts.htm
Version No.: 2; Effective From: 19/03/2012
Page 10 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
Department of Health and Ageing. Measles: National Guidelines for Public Health Units. 2009. http://www.health.gov.au/internet/main/publishing.nsf/Content/55AD336B864C7203CA257 55F000307B6/$File/measles-song.pdf Department of Health and Ageing. Pertussis: National Guidelines for Public Health Units. 2009. http://www.health.gov.au/internet/main/publishing.nsf/content/056DAAB5640EFD2FCA257 55E007629CC/$File/pertussis-song.pdf. National Health and Medical Research Council. Australian Guidelines for the Prevention and Control of Infection in Healthcare. 2010. http://www.nhmrc.gov.au/node/30290 Queensland Health. Communicable http://www.health.qld.gov.au/cdcg/default.asp Disease Control Guidelines. 2011.
Queensland Health. Foodborne Illness Outbreak Management Guidelines. 2006. http://www.health.qld.gov.au/ph/documents/cdb/31572.pdf Queensland Health Guidelines for Public Health Units. Measles. 2010. http://www.health.qld.gov.au/cdcg/index/measles.asp Queensland Health. Measles Fact Sheet. 2010 http://access.health.qld.gov.au/hid/InfectionsandParasites/ViralInfections/measles_fs.asp Queensland Health. Module 9: Outbreak Management. Public Health Nurse Communicable Disease Training Program. 2009. http://qheps.health.qld.gov.au/ph/documents/phn_cd_training/mod_9_outbreak_mgt.pdf
7.
Consultation
Infection Prevention Advisory Group ( Queensland Health) Director, Communicable Disease Prevention and Control Unit
Key stakeholders (position and business area) who reviewed this version are:
8.
Guideline Revision and Approval History
Modified by Kath OBrien Amendments authorised by Dolly Olesen Approved by Dolly Olesen
Version No. 2
Version No.: 2; Effective From: 19/03/2012
Page 11 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
ATTACHMENT 1
Duties of Chairperson Outbreak Control Team (OCT)
to declare an outbreak and convene the OCT to act as Chairperson of the OCT by leading and coordinating the response to the outbreak to endorse the outbreak management objectives and response strategy if necessary, organise an outbreak control centre and appropriate support resources where appropriate, arrange for medical examination of cases and contacts and the taking of clinical specimens where appropriate, arrange immunisation and/or chemo-prophylaxis for cases, contacts and others at risk where appropriate, notify the local Population Health Unit and CHRISP of the existence of an outbreak to ensure communication strategies are developed and implemented (see Section 4.3.4 Outbreak Control Team Communication and Reports) prepare and circulate a final report on the outbreak.
Version No.: 2; Effective From: 19/03/2012
Page 12 of 20
Printed copies are uncontrolled
ATTACHMENT 2
Sample Outbreak Log
Insert day and date ITEM NO: 1. 2. 3. 4. 5. 6. 7. 8. 9. DATE: TIME: TASK: MESSAGE: ACTION: FILE LOCATION:
Version No.: 2
; Effective From: 19/03/2012
Page 13 of 20
Printed copies are uncontrolled
ATTACHMENT 3
Checklist for Outbreak Control Team (OCT) Tasks
The principal aim of the OCT is to investigate the cause of the outbreak and to implement action to identify the source, minimise spread and prevent recurrence of the communicable disease. The following tasks must be undertaken to deal effectively with an outbreak. The step-by-step approach does not imply that each action must follow the one preceding it. In practice, some steps must be carried out simultaneously and not all steps will be required on every occasion. Outbreak Detection consider whether or not cases have the same illness and establish a tentative diagnosis determine if there is a real outbreak establish a single comprehensive case list collect relevant clinical or environmental specimens for laboratory analysis conduct unstructured, in-depth interviews of index cases conduct appropriate environmental investigation including inspection of involved or implicated premises identify population at risk identify persons posing a risk of further spread initiate immediate control measures assess the availability of adequate resources to deal with the outbreak notify the local Population Health Unit where the outbreak involves a notifiable disease or gives rise to broader public interest. Outbreak Investigation establish a case definition (clinical and/or microbiological) search for other cases collect and collate data from affected and unaffected persons using a standardised questionnaire describe cases by time, place and person form preliminary hypotheses on the cause of the outbreak make decision about whether to undertake detailed analytical studies calculate attack rates
Version No.: 2
; Effective From: 19/03/2012
Page 14 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
confirm factors common to all or most cases test and review hypotheses of the cause collect further clinical or environmental specimens for laboratory analysis ascertain source and mode of spread. Outbreak Response control the source: animal, human or environmental control the spread by: a) isolation or exclusion of cases and contacts b) treatment of cases to reduce infectious period, where possible (e.g. antivirals) c) screening and monitoring of contacts d) protection of contacts by immunisation or chemo-prophylaxis e) enhanced infection control practices by staff and visitors including cleaning and equipment decontamination procedures f) closure of premises/wards/beds monitor control measures by continued surveillance for disease declare the outbreak over. Communication consider the best means of communication with colleagues, patients and the public, including the need for an incident room and/or help-lines notify the local Population Health Unit where the outbreak involves a notifiable disease or gives rise to broader public interest consider activation of 13HEALTH ensure appropriate information is given to the public, especially those at high risk ensure accuracy and timeliness include all those who need to know use the media constructively (refer to Attachment 4 Dealing with the Media) prepare written final report (refer Section 4.3.4 Outbreak Control Team communication and Reports for items to include in the report) disseminate information on any lessons learnt from managing the outbreak. Evaluation of Response evaluate the management of the outbreak and make recommendations for the future (refer Section 4.4.4 Evaluation of Outbreak Response for possible criteria).
Version No.: 2; Effective From: 19/03/2012
Page 15 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
ATTACHMENT 4
Dealing with the Media
the Outbreak Control Team (OCT) will endeavour to keep the public and media as fully informed as possible without prejudicing the investigation and without compromising any statutory responsibilities or legal requirements at the first meeting of the OCT arrangements for dealing with the media should be discussed and agreed press statements should be prepared on behalf of the OCT by a small group including the Chairperson, Infectious Diseases Physician/Microbiologist and Media Officer press statements applicable to community associated outbreaks will normally only be released by the Media Officer, following approval by the District Chief Executive Officer of the facility. If a Media Officer is not available, the OCT will nominate an alternative spokesperson no other member of the OCT will release information to the press without the agreement of the Chairperson.
Version No.: 2; Effective From: 19/03/2012
Page 16 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
ATTACHMENT 5
Communicable Diseases of Importance
Queensland Public Health Unit - Notifiable Conditions Report Form http://www.health.qld.gov.au/ph/documents/cdb/notif_conditions_rpt.pdf Queensland Health Public Health Unit - List of all Notifiable Conditions http://www.health.qld.gov.au/ph/documents/cdb/notif_conditions_list.pdf Queensland Health Public Health Unit Contact details http://www.health.qld.gov.au/publichealthact/notifiable/phucontacts.asp Other Communicable Diseases of Public Health Importance Enterohaemorrhagic Escherichia coli (EHEC) infections viral gastroenteritis.
Other Significant Organisms of Infection Control Importance multi-resistant organisms e.g. Vancomycin Resistant Enterococci (VRE), Carbapenem-resistant Acinetobacter baumanii (CRAB or MRAB), Extended Spectrum eta-lactamase producing organisms (ESBL) Clostridium difficile infection (CDI) multi drug resistant (Pulmonary) Tuberculosis.
Version No.: 2; Effective From: 19/03/2012
Page 17 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease
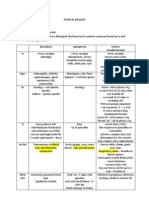
Outbreak Management Checklist
Type of Outbreak e.g. MRO, gastroenteritis, respiratory illness: Date Outbreak was reported to Infection Control: __/__/__ Reported to: Reported by: Outbreak Location/Facility: Likely Mode of Transmission: Contact Ward(s) affected: Airborne Droplet Food-borne
Water-borne
Unknown
The Outbreak Control Team should ensure the following steps are initiated as soon as possible and if initiated, completed. The order in which the tasks are undertaken may vary. if action indicated
Action
Do you have an outbreak? i.e. a higher than expected number of cases of infection with the same causative micro-organism (if known in the early stages of the outbreak) Has the source of the outbreak been identified?
if action completed
Do you need to convene the Outbreak Control Team (OCT)? Also refer to the Queensland Health Outbreak Management Guidelines Factors to be considered in the decision to convene an OCT include: (a) the type of communicable disease involved - In the case of possible healthcare associated transmission of a blood borne virus a critical incident team should be set up - see guidelines at http://www.health.qld.gov.au/chrisp/ic_guidelines/appendix_P1.pdf (b) the number of confirmed or suspected cases - large numbers of cases - two or more cases of a notifiable condition in the same ward/area, within an incubation period (c) the size and nature of the population at risk (d) the likely source (e) potential impact on service delivery - involvement of management/Executive is required to implement measures to control disease spread e.g. closure of wards/beds - involvement of more than one ward or department. Inform staff Inform all staff that a possible outbreak is occurring including advice regarding infection control measures e.g. pharmacy, messengers, volunteers, etc include supply staff and operational staff in correspondence
Version No.: 2; Effective From: 19/03/2012
Page 18 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease if action indicated
Action
if action completed
consider the need to inform visitors and patients Inform your Senior Nursing Staff on duty Inform Pathology Queensland of any additional specimen requirements
Implement additional infection control measures Ensure sufficient supplies of appropriate personnel protective equipment (PPE) is available in the affected areas e.g. mask, gloves, gowns, aprons, eyewear, as indicated by mode of transmission Isolate affected patients Display signage regarding necessary additional precautions Reinforce hand hygiene practices as appropriate Alcohol-based hand hygiene products may not be suitable for certain micro-organisms e.g. Clostridium difficile
Stop or limit further spread Consider the need to dedicate staff to affected patients e.g. in gastroenteritis outbreaks Consider the need to cohort patients with the same infection Increase cleaning frequencies in affected areas Limit transport of affected patients to essential purposes only Restrict visitors where necessary, particularly young children and people with suppressed immune systems Reinforce hand hygiene with visitors
Document the outbreak List all know cases and update information daily Include details of affected patients and staff Include details of onset date of symptoms/diagnosis for each case Notify authorities (as per OCT) Population Health notified: date: __/__/__ Communicable Disease Branch notified: date: __/__/__ CHRISP notified: date:__/__/__ Collect specimens Observe standard and appropriate additional precautions when collecting relevant specimens e.g. utilising correct PPE Collect appropriate specimens - liaise with Infectious Diseases Physician or Microbiology to determine collection method and specimen types Ensure specimens are labelled appropriately Review and up-date outbreak management plan Regularly during the outbreak
Version No.: 2; Effective From: 19/03/2012
Page 19 of 20
Printed copies are uncontrolled
Queensland Health: Guideline for the Management of Outbreaks of Communicable Disease if action indicated
Action
if action completed
Following resolution of outbreak
Outbreak management report Complete outbreak management report highlighting recommendations for preventing future occurrences
Version No.: 2; Effective From: 19/03/2012
Page 20 of 20
Printed copies are uncontrolled
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Medical MnemonicsDocument10 pagesMedical Mnemonicskenners99% (115)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Aesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Document60 pagesAesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Drhisham AttiaNo ratings yet
- FRACP Long Case NotesDocument10 pagesFRACP Long Case Notesanonymous0% (1)
- Aiims Hospital Disaster PlanDocument6 pagesAiims Hospital Disaster PlanSujatha J JayabalNo ratings yet
- De Quervain's TendinosisDocument19 pagesDe Quervain's TendinosisSze Wing LeeNo ratings yet
- Seminar ON: Birth InjuriesDocument38 pagesSeminar ON: Birth Injuriesvishnu100% (1)
- Left Knee Pain Case StudyDocument27 pagesLeft Knee Pain Case StudyREETHUNo ratings yet
- CentralVenousCatheters PDFDocument77 pagesCentralVenousCatheters PDFHarold De Leon Malang100% (1)
- Nursing Care of a Patient with AppendicitisDocument3 pagesNursing Care of a Patient with AppendicitisKeisha BartolataNo ratings yet
- Roast Chicken With Couscous & Pine Nut StuffingDocument2 pagesRoast Chicken With Couscous & Pine Nut StuffinganonymousNo ratings yet
- Personality DisordersDocument7 pagesPersonality DisordersanonymousNo ratings yet
- SIDE EFFECTS OCD AntipsychoticsDocument9 pagesSIDE EFFECTS OCD AntipsychoticsanonymousNo ratings yet
- DiabetesDocument7 pagesDiabetesanonymousNo ratings yet
- IV Fluid ChartDocument2 pagesIV Fluid Charthady920No ratings yet
- Tropical DiseasesDocument4 pagesTropical DiseasesanonymousNo ratings yet
- Diagnostic Imaging For Back Pain AFP 2004Document5 pagesDiagnostic Imaging For Back Pain AFP 2004anonymousNo ratings yet
- Trauma Management NotesDocument5 pagesTrauma Management NotesanonymousNo ratings yet
- NIH Stroke Scale Exam Order Form21Document1 pageNIH Stroke Scale Exam Order Form21anonymousNo ratings yet
- CPG Clinician Full BipolarDocument26 pagesCPG Clinician Full BipolaranonymousNo ratings yet
- Algorithm - Recognition of Dementia in Hospitalised Older AdultsDocument2 pagesAlgorithm - Recognition of Dementia in Hospitalised Older AdultsanonymousNo ratings yet
- NURS FPX 6616 Assessment 2 Summary Report on Rural Health Care and Affordable SolutionsDocument7 pagesNURS FPX 6616 Assessment 2 Summary Report on Rural Health Care and Affordable Solutionslilykevin075No ratings yet
- Gender-Dysphoric-Incongruene Persons, Guidelines JCEM 2017Document35 pagesGender-Dysphoric-Incongruene Persons, Guidelines JCEM 2017Manel EMNo ratings yet
- Cali Naturals CBDDocument7 pagesCali Naturals CBDSomya MishraNo ratings yet
- MSNHaemorrhoidsDocument17 pagesMSNHaemorrhoidsBrittany JordanNo ratings yet
- DR - Datten Bangun MSC - SPFK & DR - Tri Widyawati Msi, PHD Dept - Farmakologi & Therapeutik Fak - Kedokteran Usu MedanDocument50 pagesDR - Datten Bangun MSC - SPFK & DR - Tri Widyawati Msi, PHD Dept - Farmakologi & Therapeutik Fak - Kedokteran Usu MedanHabib Al KahfiNo ratings yet
- Complications After CXLDocument3 pagesComplications After CXLDr. Jérôme C. VryghemNo ratings yet
- Organ Systems InterviewDocument2 pagesOrgan Systems InterviewJohn Carlo MontemayorNo ratings yet
- Enzyme Disorder ProjectDocument10 pagesEnzyme Disorder Projectria wuNo ratings yet
- Faktor PICODocument1 pageFaktor PICOAlldo SaodalaNo ratings yet
- Causes of Psychiatric Illness - JAMA - 2019Document7 pagesCauses of Psychiatric Illness - JAMA - 2019ran almogNo ratings yet
- Agni Dagdha. Group-T Patients Were Treated With Indigenous Drugs and Group-C PatientsDocument14 pagesAgni Dagdha. Group-T Patients Were Treated With Indigenous Drugs and Group-C PatientsKrishnaNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanMiar QuestNo ratings yet
- 3rd Summer EvalDocument5 pages3rd Summer Evalapi-569210408No ratings yet
- Taking Medical HistoryDocument2 pagesTaking Medical HistoryDiana KulsumNo ratings yet
- Lowering Blood Pressure GuideDocument11 pagesLowering Blood Pressure GuideHilma NadzifaNo ratings yet
- Miliaria Pustulosa (Infetrop)Document11 pagesMiliaria Pustulosa (Infetrop)Muhammad mukramNo ratings yet
- Lincomycin: Drug Information: ALERT: US Boxed WarningDocument12 pagesLincomycin: Drug Information: ALERT: US Boxed WarningsadiaNo ratings yet
- Cap MRDocument4 pagesCap MRKit BarcelonaNo ratings yet
- Artículo MovilidadDocument6 pagesArtículo MovilidadMONICA DANIELA ROMERO NOCUANo ratings yet
- Kasus Istimewa - Amenorrhea PrimerDocument45 pagesKasus Istimewa - Amenorrhea PrimerMuhammad SukriNo ratings yet
- AtherosclerosisDocument7 pagesAtherosclerosisFaris Mufid Madyaputra100% (1)
- Mindful Practice: Ronald M. EpsteinDocument8 pagesMindful Practice: Ronald M. EpsteinphilosophienNo ratings yet
- Juvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16Document15 pagesJuvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16KathirNo ratings yet