Professional Documents
Culture Documents
Zeiss IOLMaster
Uploaded by
ejikieru03Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Zeiss IOLMaster
Uploaded by
ejikieru03Copyright:
Available Formats
Zeiss IOLMaster
6/29/2014 2
Optical Coherence Biometry
The Zeiss IOLMaster is a breakthrough in
measurement technology and patient care.
It is the first single instrument solution to
precisely and quickly determine axial length,
corneal curvature, and anterior chamber
depth (ACD) without ever touching the
cornea.
6/29/2014 3
Optical Coherence Biometry
The increased measurement precision and
postoperative refractive accuracy achieved
with the IOLMaster translates into enhanced
patient quality of vision and life.
6/29/2014 4
Problems with Acoustical
Biometry (ultrasound)
Inaccuracy
High Technician Variance
Many error sources (subjective)
Anesthetic required
Time consuming
Transmission of Infectious Agents
6/29/2014 5
The New Standard
The performance of the IOLMaster far
exceeds that of Conventional Biometry in the
following most important criteria:
Accuracy and Objectivity
Speed and Ease of Use
Patient Convenience
Doctor or Practice Convenience
Accuracy
The Axial Length Measurement error is smaller than
ultrasound biometry because the IOLMaster always
measures along the visual axis with proper patient
fixation.
The ultrasound biometry measurement may be off the
visual axis from -3 to +8.
When a staphyloma(elongated globe) is not coincident
with the visual axis ultrasound biometry is measuring the
off axis axial length erroneously. Staphylomas do not
affect Axial Length results with the IOLMaster.
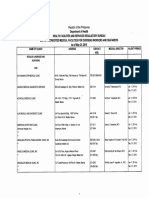
Features / Benefits
Features / Benefits
Accuracy of the Axial length measurement with the IOLMaster is better
than 0.05 mm and more around 0.03 mm. Ultrasound has at best an
accuracy of 0.1mm and typically it is 0.12 to 0.20 mm. We are at least a
factor of 2 upwards to about a factor of 5 times more accurate than
typical ultrasound.
The IOLMaster does not produce a corneal applanation error as seen in
contact ultrasound biometry. This ultrasound corneal applanation error is
a result of the subjective nature of ultrasound measurement. Technician
error may produces shorter axial lengths of about 0.2mm which
corresponds to an error in the postoperative refractive result by
approximately -0.50D.
The IOLMaster delivers reliable & repeatable readings independent of
technician technique.
6/29/2014 8
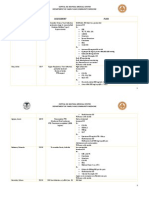
IOLMaster Repeatability Analysis
Conducted at University of Mainz in
Germany.
Determined the reproducibility of
measurements.
Intra- and Inter-Observer Variability.
6/29/2014 9
Intra-Observer Variability
1 investigator measured on each of 10 eyes
20 times Axial Length
20 times ACD
20 times Corneal Curvature
Variability found:
AL .0256 mm (this corresponds to < 0.10D
post-operatively)
ACD .0334 mm
Ks .0129mm
Significance- negligible effects on the target
refraction.
6/29/2014 10
Inter-Observer Variability
20 eyes measured by 5 investigators
Variability found:
AL .0215 mm (also < 0.10D)
ACD .0298 mm
Ks .0159 mm
6/29/2014 11
Optical Biometry is a highly
precise and reliable
measurement method that
delivers results that are
essentially independent of the
investigator (technician).
Conclusion
Ease of use
No corneal applanation/No pupil dilation.
Operational under all lighting conditions.
Measurement procedure learned very quickly
Automatic R/L eye detection.
Intuitive and familiar Windows interface.
Option of data transfer or printout.
Features / Benefits
Practice Efficiency and Patient Flow
Three measurements on a single instrument
reduces prep and exam time.
Minimal operator training.
Measure Axial Length, Corneal Curvature,
and ACD on one eye in about 1 minute.
Features / Benefits
6/29/2014 14
Features / Benefits
Patient Safety and Compliance
No anesthetic required.
A quick and easy procedure.
Non-contact technique precludes corneal
lesions and transmission of infectious agents.
Mulitple user operation
Storage of user related constants and
defaults. Each doctor (at least ten) can input
his or her own personalized lens constants for
multiple lenses (about 20) in his or her own
database.
Features / Benefits
Data for IOL power calculation
Measurement data for determination of IOL
power to implant:
Axial Length - required
Corneal Curvature - required
Anterior Chamber Depth (ACD) - optional (formula
specific)
Sources of Errors in IOL power
calculation
Measurement inaccuracy of these parameters
has been shown to contribute to deviations
from target refractions by the following
percentages:
50% of the deviations are due to an Inaccurate
Axial Length measurement
30% of the deviations are due to an Inaccurate
Corneal Curvature measurement
20% of the deviations are due to an Inaccurate
Anterior Chamber Depth measurement
6/29/2014 18
Solution
The Accuracy of the IOL Master combined with
surgeon personalization of lens constants for use
with this new measuring device minimizes these
deviations from target refractions. This leads to less
patient dependence on spectacles postoperatively
and hence an increased quality of life (better visual
outcome). Evaluation and Personalization of lens
constants is critical for any device from which
surgical technique is determined!
Description
The IOL Master is a non-contact optical
coherence biometry instrument which quickly
and accurately measures the following
parameters of the human eye:
Axial Length(AL)
Corneal Curvature(K)
Anterior Chamber Depth(ACD)
It is much, much more than a non-contact A-
scan.
Description
The Intraocular Lens (IOL) calculation window
applies these measured parameters to one of
five international IOL calculation formulas to
offer the cataract surgeon with up to 4 IOL
implant options with corresponding powers to
reach the target refraction (desired
postoperative refractive result).
Biometrical Formulas
The following empirical or geometric-optical
formulas for IOL calculation are available in
the IOL Master:
Haigis (requires optical ACD measured value)
Hoffer Q
Holladay
SRK II
SRK/T
(Note: Holladay 2 is not available on the
IOLMaster).
New Patient
6/29/2014 23
New Patient Window Tips
Always enter date of birth as mm/dd/yyyy (the
instrument will only recognize slashes / between the
numbers).
Double clicking on a patient name is the same as single
clicking on it and then clicking on new. However, do not
double click on a name unless you plan to take a
measurement on that date because the instrument will
create a file for that date as an exam date.
To review a previous examination result: 1. type in a few
letters of the patients last name in the search box. 2. Click
on the small plus icon to the left of the patients name. 3.
Double click on the desired exam date.
Screen Layout
Overview Mode
AL Measurement
Partial Coherence Interferometry(PCI)
A semi diode laser emits light (780nm) of short
coherence length that is split up into two beams
in a Michelson Interferometer. Both beams
illuminate the eye through a beam-splitting prism
and reflect at both the cornea and retina. The
light reflected from the cornea interferes with that
reflected by the retina if the optical paths of both
beams are equal.
AL Measurement
PCI continued
The interference is detected by a photodetector.
The signals are amplified, filtered and recorded
as a function of the position of the interferometer
mirror(high accuracy). From this mirror the
system determines the axial length as the path
difference between the cornea and the retinal
pigment epithelium (RPE).
6/29/2014 28
6/29/2014 29
Retinal Structures
The axial length as measured with a ultrasound
biometrical instrument is that distance from the
cornea to the inner limiting membrane (ILM). Since
the IOLMaster measures to the RPE it is important
to know that the system internally takes into account
the distance difference between the ILM and the
RPE. Thus the displayed AL values with the
IOLMaster are directly comparable to those
measured acoustically using the immersion
ultrasound technique.
AL Measurement Alignment
AL Measurement Tips
Instruct the patient to look at the red fixation light.
Note: in all other modes the fixation light is yellow.
Take 5 measurements (maximum allowable is 20 /
eye / day)
If error measurements occur- keep trying! (20
chances)
If unsuccessful: Vary the location of fixation light
within green circular cross hair on display to find
window of opportunity through the opacity.
AL Measurement Tips
After each measurement a new average is
usually displayed. When one or more
measurements varies by >0.1mm from the
mean no average will be displayed, but the
word Evaluate! This alerts the operator to
evaluate the AL measurement results(more
later).
AL Measurement Tips
6/29/2014 34
AL Setings
The AL Settings may be selected for
conversion to proper axial length for different
eye types.
May be selected before or any time after the
measurement.
The default setting after switching eyes is
Phakic.
AL Measurement
Technical Data
Measuring Range 14 - 39 mm
Accuracy on Test Eye 0.01mm
Display Resolution 0.01mm
Reproducibility on eye <0.03mm
This reproducibility corresponds to a mean
postoperative error < 0.10 D.
K Measurement
Autokeratometer-The Corneal Curvature is
determined by measuring the distance
between 6 reflected IR light images. A CCD
camera captures the image.
Recommend blinking to replenish tear film to
improve image quality.
The displayed result is an average of 5
measurements taken within 0.5 seconds.
K Measurement
With each new measurement the previous
result is overwritten.
For measurement errors as well as limitations
(dry eye, corneal scarring) see Tips for
keratometer measurement in users manual.
K Measurement
Alignment: Focus the 6 peripheral lights so that they are
lying concentric between the two auxiliary circles on the
display. The center point is used only for alignment and
is usually dimmer and smaller than the peripheral lights.
K Measurement
K Measurement
In the Options menu it is necessary under the
Setup then Program Settings submenu to
input the Refractive Index of the practice
Keratometer(see owners manual). In the U.S.
this value is typically 1.3375. This value is
used to convert corneal radii into refractive
powers(D).
K Measurement
Technical Data (Human Eye)
Measuring Range of Cornea 33-67D
(5-10mm)
Astigmatism Range up to 10D
Repeatability 0.02mm
Display Resolution 0.01mm
Diameter of measuring area < 3.0 mm
ACD Measurement
The ACD is determined as the distance
between the optical sections of the cornea
and the crystalline lens produced by lateral
slit illumination of approximately 30 to the
optical axis. Facilitated via a CCD Camera.
The lateral slit illumination flickers during
measurement and it always originates from
the temporal field of the eye being measured.
ACD Measurement
With each measurement 5 readings are taken
and displayed along with their average on
the monitor. After each measurement there is
a 15 second processing time( have patient sit
back to avoid excess illumination).
The K Measurement must be done prior to
the ACD Measurement. If K Readings were
not possible with this instrument they must be
entered manually prior to the ACD
Measurement.
ACD Measurement Alignment
1. Focus the fixation point image in screen rectangle by
making it small with sharp borders . It should be
near the optical section of the lens but not in it.
2. The corneal optical section should not be disturbed
by reflections
3. The anterior crystalline lens is optimally visible.
Note: Due to system design the corneal section is
unclear. See handout Tips.
ACD Measurement
ACD Measurement
Technical Data (Human Eye)
Measuring Range 1.5 to 6.5 mm
Display Resolution 0.01 mm
Repeatability 0.1 mm
Evaluation of AL Measurements
The IOL Master is capable of resolving fine
structures on the fundus of the eye. Depending on
the anatomical conditions of the measured eye, it
may also happen that the measuring beam
produces interference not only at the RPE but at the
inner limiting membrane of the retina and/or at the
choroid. Verification is necessary when multiple
peaks are present and/or significant variance
between results exists such that Evaluate! is
present instead of an average value.
Evaluation of AL Measurement
The results of AL measurements are to be
interpreted on the basis of signal-to-noise
ratio(SNR) and the appearance of the graphs.
The SNR value is an indicator of the quality of the
measurement.
A SNR value < 2.0 may be due to:
Strong ocular opacities, poor fixating patients, high
refractive error( > 6D), pathological retinal changes.
(Note: In some case of high refractive error,
measurement through the patients spectacle
lenses may be needed).
SNR Values
If SNR is > 2.0 then the measured value is
valid
If SNR is in the range 1.6 to 2.0 then the
measured value is not reliable or borderline
(!). It still may be usuable!
If SNR is < 1.6 then the measured value is
unusable (Error)
Evaluation of AL Measurement
AL Graph Analysis
The measuring cursor (circle) is automatically placed on the
center of the signal peak with the highest amplitude. By
variance among measurement values in a series such that
no average is present and Evaluate! is present, the graphs
must be analyzed to determine if the signal peak is the true
axial length( RPE ) or if another fundus structure has
produced the highest peak (and hence the wrong axial
length). To achieve this, one must zoom in on the graph. If a
structure other than the RPE has the circle above it that
result may be 1) deleted or 2) corrected by shifting the circle
above the RPE (manipulation). When the cursor has been
shifted the result will always have an asterisk* next to it
to denote its manipulation. See users manual to learn how
to shift cursor.
For optimal AL graph analysis
use the zooming feature:
Move the arrow cursor on the length axis (x-
axis) to the position that should be in the
center of the zoomed image.
Press the left mouse button up to 4 times for
sequential zooming.
Press the right mouse button to return to
original view of graph.
Triple peak
Double peak with RPE > ILM
(Correct Axial Length Value)
Distance between peaks is .15 to .35 mm.
Double peak with ILM > RPE
(Incorrect Axial Length Value)
AL value would be .15 to .35 mm shorter than
other values from that eye. Delete reading or
move cursor to RPE (manipulate).
Triple peak ILM, RPE, Choroid
(Incorrect Axial Length Value)
IOL Calculation
IOL Database
Clinical Evaluation
The following specialists have overwhelmingly
endorsed the IOLMaster:
Dr. Holladay (Houston, TX)
Dr. Wallace (Alexandria, LA)
Dr. Hoffer (Santa Monica, CA)
Dr. Haigis (Germany)
Dr. Fine (Eugene, OR)
Dr. Gills (Tarpon Springs, FL)
6/29/2014 60
Limitations
Haigis showed that between 5-10% of patients are not
measurable with the IOL Master.
tremor or poor fixating patients
significant ocular opacities (scars, vitreous hemorrhages,
dense nuclear or posterior subcapsular cataracts )
Corneal ablations
Visual Acuity alone is not predictive of measurement
capability.
Better said: 90-95% of patients will have a more precise
postoperative refractive result because of the accuracy and
ease of use of the IOLMaster. Practice efficiency will be
greatly improved using the IOLMaster.
You might also like
- Ofw Clinic May202015Document14 pagesOfw Clinic May202015ejikieru03No ratings yet
- AnatomyDocument18 pagesAnatomyeNo ratings yet
- ADocument1 pageAejikieru03No ratings yet
- PB Guangzhou 2012Document6 pagesPB Guangzhou 2012ejikieru03No ratings yet
- MS MriDocument22 pagesMS Mriejikieru03No ratings yet
- Instilling Purpose in Your ChoirDocument3 pagesInstilling Purpose in Your Choirejikieru03No ratings yet
- 47.taxability of Productivity Incentive Bonuses.07.10.08.GACDocument2 pages47.taxability of Productivity Incentive Bonuses.07.10.08.GACEumell Alexis PaleNo ratings yet
- FM Cases OpdDocument13 pagesFM Cases Opdejikieru03No ratings yet
- Uy CheatsDocument10 pagesUy Cheatsejikieru03No ratings yet
- Skin Physical ExamDocument10 pagesSkin Physical ExamVenkatesan VidhyaNo ratings yet
- Our Proforma Invoice Mbli/04/07/M-891: FOR: Our Lady of Mercy General HospitalDocument3 pagesOur Proforma Invoice Mbli/04/07/M-891: FOR: Our Lady of Mercy General Hospitalejikieru03No ratings yet
- MSDocument8 pagesMSejikieru03No ratings yet
- Equipment For Ophthalmology: FOR: Amang Rodriguez Medical Center Attention: Roland L. Cortez, M.DDocument2 pagesEquipment For Ophthalmology: FOR: Amang Rodriguez Medical Center Attention: Roland L. Cortez, M.Dejikieru03No ratings yet
- Proforma Invoice 15Document5 pagesProforma Invoice 15ejikieru03No ratings yet
- MS Definition and AnatomyDocument9 pagesMS Definition and Anatomyejikieru03No ratings yet
- FOR: Paulino J. Garcia Mem. Medical Center: Our Proforma Invoice Mbli/04/06/M-804Document3 pagesFOR: Paulino J. Garcia Mem. Medical Center: Our Proforma Invoice Mbli/04/06/M-804ejikieru03No ratings yet
- Nueva Ecija Doctors Hospital: Our Proforma Invoice Mbli/04/11/M-1445Document3 pagesNueva Ecija Doctors Hospital: Our Proforma Invoice Mbli/04/11/M-1445ejikieru03No ratings yet
- Proforma Invoice 15Document5 pagesProforma Invoice 15ejikieru03No ratings yet
- Proforma Invoice 7Document3 pagesProforma Invoice 7ejikieru03No ratings yet
- Proforma Invoice 14Document2 pagesProforma Invoice 14ejikieru03No ratings yet
- Proforma Invoice 13Document3 pagesProforma Invoice 13ejikieru03No ratings yet
- Proforma Invoice 14Document2 pagesProforma Invoice 14ejikieru03No ratings yet
- Proforma Invoice 11Document3 pagesProforma Invoice 11ejikieru03No ratings yet
- FOR: Ospital NG Maynila and Medical Center: Our Proforma Invoice Mbli/04/06/M-797Document4 pagesFOR: Ospital NG Maynila and Medical Center: Our Proforma Invoice Mbli/04/06/M-797ejikieru03No ratings yet
- Proforma Invoice 10Document3 pagesProforma Invoice 10ejikieru03No ratings yet
- Proforma Invoice 3Document6 pagesProforma Invoice 3ejikieru03No ratings yet
- Proforma Invoice 8Document3 pagesProforma Invoice 8ejikieru03No ratings yet
- Proforma Invoice 2Document2 pagesProforma Invoice 2ejikieru03No ratings yet
- Proforma Invoice 4Document3 pagesProforma Invoice 4ejikieru03No ratings yet
- Proforma InvoiceDocument2 pagesProforma Invoiceejikieru03No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- PhotographyDocument47 pagesPhotographyKhris Jann Tabag100% (1)
- Scanning Probe MicrosDocument26 pagesScanning Probe MicrosthomasNo ratings yet
- Fischerscope X-Ray Xdal 237Document4 pagesFischerscope X-Ray Xdal 237PO Hsien YUNo ratings yet
- One Sky ManualDocument12 pagesOne Sky ManualDevin ShivelyNo ratings yet
- Implementation Notes: 2.1. Link CalculationDocument8 pagesImplementation Notes: 2.1. Link CalculationpanjeduNo ratings yet
- Top Physical, Biological, Ergonomic and Chemical HazardsDocument274 pagesTop Physical, Biological, Ergonomic and Chemical HazardsrwerwerwNo ratings yet
- General AwarenessDocument159 pagesGeneral AwarenessNiladri GoswamiNo ratings yet
- PSC 2014 April 15 PDFDocument24 pagesPSC 2014 April 15 PDFRemyanair NairNo ratings yet
- Basic Physics 2 WEEK1 26022016Document36 pagesBasic Physics 2 WEEK1 26022016SERAPHINENo ratings yet
- Wave Optics ExercisesDocument16 pagesWave Optics ExercisesRitesh BNo ratings yet
- Philips G3 PDFDocument19 pagesPhilips G3 PDFAndreRibeiro DroneNo ratings yet
- Measurement of Average Sky Glow by Digital CameraDocument6 pagesMeasurement of Average Sky Glow by Digital CameraAbhijit Kar GuptaNo ratings yet
- Electromagnetic Spectrum Physics o LevelDocument4 pagesElectromagnetic Spectrum Physics o LevelDark VariantNo ratings yet
- Fiel Guide To Geometrical Optics - JJhon GreivenkampDocument132 pagesFiel Guide To Geometrical Optics - JJhon Greivenkampwilliasj100% (6)
- Alroy Feed BrochureDocument12 pagesAlroy Feed BrochureNur FaiqahNo ratings yet
- Applying the Zone System to Digital PhotographyDocument5 pagesApplying the Zone System to Digital PhotographyElsonB100% (1)
- T223-0583 - 16 - EN12368-2015 300mm Colour FLDocument29 pagesT223-0583 - 16 - EN12368-2015 300mm Colour FLarainzada807No ratings yet
- List of vehicle horns and relaysDocument460 pagesList of vehicle horns and relaysSunesh KumarNo ratings yet
- Przenieś Rozwiązania Na Kartę Odpowiedzi!: MJA-1RDocument3 pagesPrzenieś Rozwiązania Na Kartę Odpowiedzi!: MJA-1RVassos Serghiou SrNo ratings yet
- Lecture 1Document53 pagesLecture 1Aalim KhanNo ratings yet
- Grade 7 MicroscopeDocument27 pagesGrade 7 MicroscopeRamyRamia ElzantNo ratings yet
- Phase-Shift Fizeau Interferometer in Presence of VibrationDocument12 pagesPhase-Shift Fizeau Interferometer in Presence of VibrationMircea BujorNo ratings yet
- Canon EOS SystemDocument33 pagesCanon EOS SystemArnaldo de Moraes Pereira100% (15)
- X Ray Diffraction Safety InformationDocument48 pagesX Ray Diffraction Safety Informationrenjith2017100% (1)
- Axorad: Radiation Resistant Cables For Scientific & Nuclear ApplicationsDocument50 pagesAxorad: Radiation Resistant Cables For Scientific & Nuclear ApplicationsFrancesca TeocoliNo ratings yet
- BVOC Hospital EquipmentDocument72 pagesBVOC Hospital EquipmentYagnesh MakwanaNo ratings yet
- Product Overview LaserDocument45 pagesProduct Overview LaserRoman JambrekNo ratings yet
- Chapter 14: Geometric Optics: CK-12 Physics Concepts - Intermediate Answer KeyDocument7 pagesChapter 14: Geometric Optics: CK-12 Physics Concepts - Intermediate Answer KeyRegine AngelesNo ratings yet
- LP1 Reflection of Light in Plane MirrorsDocument11 pagesLP1 Reflection of Light in Plane MirrorsAbet Laborte100% (4)
- 2013 CCTV CatalogDocument295 pages2013 CCTV CatalogEPCOMUSANo ratings yet