Professional Documents
Culture Documents
CVS Examination Edited
Uploaded by
Thilak JayalathOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CVS Examination Edited
Uploaded by
Thilak JayalathCopyright:
Available Formats
Examination of
Cardiovascular
System
First impression
Inherited syndromes
Down's syndrome (PDA, ASD & VSD)
Marfan's syndrome (aortic dissection,
valve disease)
Turner's syndrome (aortic coarctation
& aortic stenosis)
Ankylosing spondylitis
(aortic regurgitation)
Acromegaly
(hypertension &
cardiomegaly)
Other syndromes
Downs syndrome
Marfan s
syndrome
Turner s syndrome
Turner s syndrome
Acromegaly
Acromegaly
General
Examination
Breathlessness
In pain
Febrile
Pallor
Xanthelesma
Xanthelesma
Cleft ear lobes
Central cyanosis
Dental care
Thyroid enlargement
Central cyanosis
Clubbing of the fingers
Splinter heamorrhages
Splinter haemorrhages
Oslers nodes
Janeways lesions
Ankle oedema
Sacral oedema
Pulse
Presence or absence
Rate
Rhythm
Character
Presence of bruits
Jugular venous pulse
Jugular venous pressure
The internal jugular vein provides
information about right atrial and right
ventricular function
The jvp can be discriminated from the carotid pulse
because:
It cannot be palpated
It has a complex wave form; it is usually seen to flicker
twice within each cardiac cycle
It moves on respiration, normally decreasing on inspiration
and rising on expiration
Mild pressure applied to the base of the neck obliterate its
pulsations
Mild pressure applied over the liver will expel more blood
into the right side of the heart and elevate the jvp, a
positive hepato-jugular reflex
Jugular venous wave pattern
The jvp is described in terms of:
Height
character
The height of the jvp is expressed as the
vertical distance from the manubriosternal
angle to the maximum height of pulsations
in the internal jugular vein with the patient
semi-recumbent at an angle of 45 degrees
It is normally less than 3 cm.
This equates to a right atrial pressure of 8
cm of water as in this position, the
manubriosternal angle is about 5 cm
above the centre of the right atrium
Causes of a raised jvp
increased right ventricular filling pressure
obstruction of blood flow from the right atrium
to the right ventricle
superior vena caval obstruction
positive intrathoracic pressure
Abnormal waves
Abnormally large a waves indicate
increased resistance to right atrial emptying
from right ventricular hypertrophy, as in
severe pulmonary stenosis, or tricuspid
stenosis.
Abnormal waves
A waves are absent in atrial fibrillation,
since coordinated atrial contraction is
necessary to produce them,
Abnormal waves
Cannon waves are very large a waves that
occur when the right atrium contracts against a
closed tricuspid valve.
They occur irregularly in complete heart block
and ventricular tachycardia, conditions that
are characterised by atrioventricular
dissociation with random occasional
simultaneous atrial and ventricular
contractions.
An exaggerated x descent indicates that
blood is being ejected from a restricted
pericardial cavity, for example, because
of cardiac tamponade or constrictive
pericarditis without calcification.
A slow y descent may be seen in
tricuspid stenosis and right atrial
myxoma.
Examination of the
precordium
Scars,
The midline scar of a sternotomy
The left lateral scar of a mitral
valvotomy
Deformity
Pacemaker
Visible apex beat or other pulsation
Inspection
Pectus excavatum
Palpation
Apex beat
Parasternal haeve
Palpable heart sounds
Plapable murmurs
Apex beats different types
Sustained or heaving apex beat is
caused by pressure overload
aortic stenosis,
severe hypertension.
Apex beats different types
Tapping apex beat seen in
Mitral stenosis
Apex beats different types
Thrusting displaced apex beat is
caused by volume overload: an
active large stroke volume ventricle
Aortic regurgitation
Mitral regurgitation
Left to right shunts.
Apex beats different types
Double or triple impulse occur in
Hypertrophic obstructive
cardiomyopathy
Apex beats different types
An impalpable apex beat
Obesity
Overinflated chest
Pericardial effusion
Dextrocardia
Apex beat
Parasternal heave is detected by
placing the heel of the hand over
the left parasternal region. In the
presence of a heave the heel of the
hand is lifted off the chest wall with
each systole.
Parasternal haeve
Parasternal heave is caused by:
Right ventricular enlargement
Severe left atrial enlargement
which pushes the right ventricle
forwards
Thrill
These are palpable murmurs
They always indicate an organic defect
The area where the thrill is felt strongest
gives clues as to the aetiology of the thrill
Thrills may be
Systolic or diastolic:
Best felt site suggest the oetiology
Systolic:
Apex mitral incompetence
at 3rd or 4th interspace vsd
At base on right aortic stenosis
at base on the left pulmonary stenosis
Below left clavicle - pda
Diastolic:
Apex mitral stenosis
Accurate and sensitive
auscultation of the
praecordium requires
experience
Location of heart valves
Auscultation should begin in the mitral
region:
Use the bell initially to detect the low
frequency sounds of mitral stenosis or a
third heart sound
Use the diaphragm to detect the higher
frequency sounds of mitral incompetence
or a fourth heart sound
Using the bell and diaphragm, listen
in the following locations
Tricuspid area
Pulmonary area
Aortic area
Never forget to
Auscultate over the mitral
area in left lateral position in
expiration with the bell to find
mid diastolic murmur in mitral
stenosis
Never forget to
Auscultate over the lower
left sternal edge in
expiration , in seated and
bent forward position, with
the diaphram to find early
diastolic murmur in aortic
incompetence
Heart sounds
There are two major groups of heart
sounds
They are classified according to their
mechanism,
Valvular
Ventricular filling
Valve sounds
These include:
First heart sound
Second heart sound
ejection sounds
opening snaps
The first heart sound is caused by
the closing of the mitral valve
and the closing of the tricuspid
valve
It is heard loudest at the apex.
Possible causes of a soft first heart
sound include
Mitral regurgitation
low blood pressure,
rheumatic carditis
severe heart failure
left bundle branch block
Loud first sounds
A loud first heart sound occurs when the
leaflets are wide open at the end of
ventricular diastole and shut forcefully at
the beginning of ventricular systole.
Causes of loud first heart sound
Atrial fibrillation
short diastole tachycardia
Atrial premature beat
Mitral stenosis where high left atrial
pressure delays mitral valve closure
If the blood flow from atria to ventricles
varies from one beat to the next, then
the intensity of the first heart sound will
change accordingly
Causes include
Varying duration of diastole
Complete atrioventricular block
A soft, or absent, a2 is heard in:
Poorly mobile cusps
calcification as occurs in some forms of
aortic stenosis
dilatation of the aortic root - syphilitic
aortitis
A soft, or absent, p2 is heard in:
Pulmonary stenosis
Loud second heart sounds can be loud
a2 or a loud p2.
Loud a2 occurs in systemic hypertension
where there is a dilated proximal aorta
A loud p2 is heard in pulmonary
hypertension
Splitting of second heart sound
A2 and p2 separate on inspiration
(P2 following a2)
This is because of the increased right
ventricular stroke volume that occurs as
the result of increased venous return
The second heart sound is widely split if
there is an early a2 or if the p2 is
delayed.
Early A2 can occur in
Mitral regurgitation
Ventricular septal defect
Delayed p2
Possible causes include :-
Right bundle branch block
Pulmonary stenosis
Atrial septal defect
Fixed splitting
Splitting of seond heart sound in
both inspiration and expiration
Reversed splitting
In this condition, p2 occurs before a2
On expiration, a2 is delayed such that it
occurs after p2
Inspiration causes p2 to be delayed and
the split is diminished.
Possible causes of a delayed a2
Left bundle branch block
systolic hypertension
severe aortic stenosis or hocm
patent ductus arteriosus
left heart failure
Ejection clicks
These are caused by the opening of the
aortic and pulmonary valves.
These sounds are high pitched and often
described as clicky.
They occur in early systole and are best
heard with a rigid diaphragm chest piece.
Opening snaps
In certain pathological states the av
valves open more rapidly than normal,
this results in an audible opening snap.
A mitral opening snap may be
caused by:
Mitral stenosis with a mobile valve
Rapid mitral flow causes a soft snap in left
to right shunts such as
Vsd or pda.
Severe mitral regurgitation
A tricuspid opening snap is rare and may
be caused by:
Rheumatic stenosis
Atrial septal defect with increased
tricuspid flow
Filling sounds
These sounds are of much lower frequency than
the valve sounds and may be difficult to hear.
They are best heard with the bell gently applied
to the chest and are described as a dull thud
becoming palpable when loud.
Ventricular filling sounds include:
Rapid filling (third)
Atrial (fourth)
Third heart sound
This heart sound is caused by rapid
ventricular filling in early diastole.
The third sound is normally audible in
children, with the intensity diminishing
with age.
The third heart sound becomes
inaudible (but recordable) in normal
subjects in middle age with increasing
ventricular stiffness.
Fourth heart sound
The fourth heart sound is due to atrial
contraction inducing ventricular filling
towards the end of diastole.
They are never audible in normal
subjects.
A fourth heart sound is the result of
powerful atrial contraction filling an
abnormally stiff ventricle.
Left atrial heart sound is maximal at the
apex, with possible causes including:
Left ventricular hypertrophy
fibrotic left ventricle
hypertrophic cardiomyopathy
Right atrial heart sound is maximal at the
lower left sternal edge and on inspiration.
This may occur in
Right ventricular hypertrophy
Murmurs
Heart murmurs are caused by
turbulent blood flow through
valves or ventricular outflow
tracts
Characteristics of heart murmurs
Timing
Duration
Character and pitch
Intensity
Location
Radiation
Murmurs are recorded in six gradations:
1/6 murmur is just audible by an expert in optimal
conditions
2/6 is quiet
3/6 is moderately loud
4/6 is markedly loud , accompanied by a thrill
5/6 is very loud with a thrill
6/6 is audible without a stethoscope
With reference to valvular lesions
Systolic murmurs imply incompetence of
atrioventricular valve or stenosis/sclerosis
of semilunar valve.
Diastolic murmurs imply stenosis of
atrioventricular valve or incompetence of
semilunar valve
Left ventricular ejection murmurs are
maximal at the aortic area, lower left
sternal edge and apex.
Possible causes include:
Aortic stenosis
Hypertrophic obstructive
cardiomyopathy
aortic cusp sclerosis
Ejection systolic murmur maximal over
the aortic area:
Aortic stenosis
Aortic sclerosis
Coarctation of the aorta
Hypertrophic cardiomyopathy
Ejection systolic murmur maximal over
the pulmonary area:
Innocent
pulmonary stenosis
pulmonary hypertension
atrial septal defect
Pansystolic murmurs
Pansystolic murmurs occur throughout
systole
Caused by:
Mitral regurgitation
Ventricular septal defect
tricuspid regurgitation
Diastolic murmurs
Early diastolic murmurs
Mid-diastolic murmurs
Early diastolic murmurs
Aortic regurgitation - maximal at the 4th
interspace below the aortic valve.
Maximal if the patient leans forwards.
Radiates to the back.
Pulmonary regurgitation - maximal about
the third left space.
Mid diastolic murmurs
Mitral stenosis - maximal at the apex with
the patient inclined to the left. The murmur
begins after the opening snap. The
murmur is long if severe and short if mild.
Tricuspid stenosis - maximal at the lower
left sternal edge. The murmur is increased
by inspiration.
A murmur mimicking mitral stenosis may
occur when there is greatly increased
flow across the mitral valve.
This may occur in
mitral regurgitation,
Ventricular septal defect
Patent ductus arteriosus
Continuous murmur
These occur when there is a
communication in the circulation with a
continuous pressure gradient throughout
the cardiac cycle.
Continuous murmurs are often maximal in
late systole
Causes of a continuous murmur include:
Patent ductus arteriosus
aortic sinus of valsalva aneurysm rupturing into
the right heart
pulmonary arteriovenous communications
Bronchial artery anastomosis in pulmonary
atresia
Artificial ducts
prosthetic valve
Venous hum
Innocent murmurs
Many babies and children have heart
murmurs in the absence of any structural
abnormality
If a murmur has any of the following
characteristics then it probably is not innocent:
Pansystolic
diastolic
loud or long
associated with a thrill or cardiac symptoms
.`
Some hints concerning listening for
murmurs:
Time the cardiac cycle by palpating one of the
patient's carotid arteries
The bell is good for hearing low-pitched sounds
e.G. Mitral stenosis. It should be applied very
gently to the skin
The diaphragm is good for listening to high
pitched mumurs e.G. Aortic regurgitation
Some hints concerning listening for
murmurs:
Left heart murmurs are louder in expiration
Right heart murmurs are louder in
inspiration
Exercise makes a mitral stenotic murmur
louder
END
You might also like
- Priscilla's Medicine With Addon FinalDocument432 pagesPriscilla's Medicine With Addon FinalLee100% (1)
- Abnormal Heart Sounds: First Heart Sound (S)Document4 pagesAbnormal Heart Sounds: First Heart Sound (S)Faris Mufid MadyaputraNo ratings yet
- Heart Failure: Low Output HF High Output HFDocument7 pagesHeart Failure: Low Output HF High Output HFJake BurrNo ratings yet
- Magic Book DR Nikita 2.0 OnlineDocument263 pagesMagic Book DR Nikita 2.0 OnlineDinesh MorNo ratings yet
- S1 and S2: Valves) at The Start of The Systolic Contraction of The VentriclesDocument10 pagesS1 and S2: Valves) at The Start of The Systolic Contraction of The VentriclesCHARIEMAE CA�AZARESNo ratings yet
- Differential Diagnosis of Valvular Heart DiseaseDocument10 pagesDifferential Diagnosis of Valvular Heart DiseaseAbhisek ChatterjeeNo ratings yet
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Cardiovascular: Surfaces of The HeartDocument6 pagesCardiovascular: Surfaces of The HeartironNo ratings yet
- Arrhythmia S: DRDM KillingoDocument95 pagesArrhythmia S: DRDM KillingoMalueth Angui100% (1)
- Heart Sounds: Mitral Regurgitation Congestive Heart FailureDocument6 pagesHeart Sounds: Mitral Regurgitation Congestive Heart FailurecindyNo ratings yet
- Cardiovascular System PDFDocument182 pagesCardiovascular System PDFXochitl ZambranoNo ratings yet
- Endocrine Notes - All in One FileDocument182 pagesEndocrine Notes - All in One FilekjNo ratings yet
- Heart SoundDocument2 pagesHeart SounddamarisapNo ratings yet
- Cardiovascular Examination: Andi Wahjono Adi, MD, FihaDocument34 pagesCardiovascular Examination: Andi Wahjono Adi, MD, FihaAmira FRNo ratings yet
- Examination of Cardiovascular SystemDocument24 pagesExamination of Cardiovascular SystemThilak JayalathNo ratings yet
- Circulatory SystemDocument2 pagesCirculatory SystemcatchivanNo ratings yet
- Evaluation of Chest Pain in Primary Care Patients-AAFPDocument3 pagesEvaluation of Chest Pain in Primary Care Patients-AAFPnouval_iqbalNo ratings yet
- Suatu Alat Laboratoris Alat Bantu DiagnosisDocument78 pagesSuatu Alat Laboratoris Alat Bantu DiagnosisAnonymous 3LwVkUsdNo ratings yet
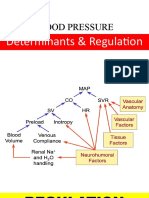
- Short and Long Term Regulation and Determinants of BPDocument90 pagesShort and Long Term Regulation and Determinants of BPDan Tristam MicabaloNo ratings yet
- Advanced Cardiac Life SupportDocument37 pagesAdvanced Cardiac Life SupportRoy Acosta GumbanNo ratings yet
- Basic ECG Interpretation GuideDocument60 pagesBasic ECG Interpretation GuideLexadkNo ratings yet
- Physio Coursepack 2016Document282 pagesPhysio Coursepack 2016Amanda KimNo ratings yet
- Vital SignsDocument2 pagesVital SignsVSNo ratings yet
- OutputDocument12 pagesOutputzenishzalamNo ratings yet
- Aortic StenosisDocument20 pagesAortic Stenosisvasarhely imolaNo ratings yet
- Cardio Day 3: Hypertension, Hyperlipidemia, Arteriosclerosis, Ischemic Heart DiseaseDocument24 pagesCardio Day 3: Hypertension, Hyperlipidemia, Arteriosclerosis, Ischemic Heart DiseaseMikeNo ratings yet
- Mark M Calban MD MPM-HSDDocument58 pagesMark M Calban MD MPM-HSDZllison Mae Teodoro Mangabat100% (1)
- Kuliah Ekg UnswagatiDocument75 pagesKuliah Ekg UnswagatiiikNo ratings yet
- Adrenergic Agonist and AntagonistDocument35 pagesAdrenergic Agonist and AntagonistFirjat AfiataNo ratings yet
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- Cardiac Anatomy and Phvsiologv A Review - Aorn800Document16 pagesCardiac Anatomy and Phvsiologv A Review - Aorn800Citra Ayu ApriliaNo ratings yet
- Heartbeat Irregularities ExplainedDocument5 pagesHeartbeat Irregularities ExplainedKayelyn-Rose Combate100% (1)
- Hemodynamic disturbances and their pathological effectsDocument74 pagesHemodynamic disturbances and their pathological effectsAmmar Bany AtaNo ratings yet
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationDocument28 pagesCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- Chap253-Heart Failure ManagementDocument42 pagesChap253-Heart Failure ManagementDoctor CastleNo ratings yet
- Cardiac Output and Hemodynamic MeasurementDocument29 pagesCardiac Output and Hemodynamic Measurementdeepa100% (1)
- Blood Vessel (Student)Document148 pagesBlood Vessel (Student)Jerkin Razhed PostanesNo ratings yet
- VALVULAR HEART DISEASE GUIDEDocument69 pagesVALVULAR HEART DISEASE GUIDEAbanoub AwadallaNo ratings yet
- Core V - Cardiovascular CoreDocument35 pagesCore V - Cardiovascular CoreMatthew LeiNo ratings yet
- STRUCTURE AND FUNCTION OF THE HEARTDocument16 pagesSTRUCTURE AND FUNCTION OF THE HEARTPkernNo ratings yet
- Vasopressors in ShockDocument8 pagesVasopressors in ShockOrion JohnNo ratings yet
- Adrenergic Agonists: Classification and UsesDocument44 pagesAdrenergic Agonists: Classification and UsesAneeza AhmadNo ratings yet
- Functional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionDocument186 pagesFunctional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionBery Agana F. PurbaNo ratings yet
- Mechanical Properties of The Heart IDocument30 pagesMechanical Properties of The Heart ISeba W WolfNo ratings yet
- พี่พงษ์ติวcardioDocument79 pagesพี่พงษ์ติวcardioRapid Medicine67% (3)
- Principles of ECGDocument11 pagesPrinciples of ECGDeinielle Magdangal RomeroNo ratings yet
- L9 PDFDocument22 pagesL9 PDFMiles HuiNo ratings yet
- ECG Learning ModulesDocument150 pagesECG Learning ModulesdodiNo ratings yet
- Cardiac EmergenciesDocument38 pagesCardiac Emergenciesnurasia oktianiNo ratings yet
- Systolic Dysfunction:: Types of Heart FailureDocument13 pagesSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaNo ratings yet
- Vascular System: - Arteries Arterioles - Capil ExchDocument35 pagesVascular System: - Arteries Arterioles - Capil ExchMikaelle GasparNo ratings yet
- Acid-Base Disorders NotesDocument10 pagesAcid-Base Disorders NotesLovely100% (1)
- Cardiology Summary PDFDocument62 pagesCardiology Summary PDFSyamsuriWahyuNo ratings yet
- ECG Interpretation in One PageDocument2 pagesECG Interpretation in One PageRyan AycockNo ratings yet
- Arrhythmias: Sing Khien Tiong Gpst1Document34 pagesArrhythmias: Sing Khien Tiong Gpst1preethi preethaNo ratings yet
- Regulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowDocument20 pagesRegulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowShveta MahajanNo ratings yet
- Beta-Adrenergic BlockersDocument14 pagesBeta-Adrenergic BlockersAnonymous NVAWeVWNo ratings yet
- UTIDocument17 pagesUTIBongkotchakorn Mind PhonchaiNo ratings yet
- Arrhythmia & Anti-Arrhythmic DrugsDocument49 pagesArrhythmia & Anti-Arrhythmic DrugsNitesh SinghNo ratings yet
- ECG ReviewDocument146 pagesECG ReviewThea DinoNo ratings yet
- Examination of Cardiovascular SystemDocument24 pagesExamination of Cardiovascular SystemThilak JayalathNo ratings yet
- Acute nephritic syndrome clinical features causes and managementDocument3 pagesAcute nephritic syndrome clinical features causes and managementThilak JayalathNo ratings yet
- Regulate Extracellular Fluid Kidney FunctionDocument3 pagesRegulate Extracellular Fluid Kidney FunctionThilak JayalathNo ratings yet
- Kidney at A GlanceDocument120 pagesKidney at A GlanceMayer Rosenberg100% (2)
- AuscultationDocument19 pagesAuscultationDrVishal YadavNo ratings yet
- Maternal changes during pregnancyDocument38 pagesMaternal changes during pregnancyHei KamuNo ratings yet
- Osce ChecklistDocument11 pagesOsce Checklistgemgem06No ratings yet
- Raju B Soma Ed Clinical Methods in Cardiology PDFDocument522 pagesRaju B Soma Ed Clinical Methods in Cardiology PDFAshishsanjay Munoli0% (1)
- Liu 2016Document34 pagesLiu 2016Arina AndriesNo ratings yet
- Physical Examination in PaediatricsDocument162 pagesPhysical Examination in PaediatricsUsman Ali100% (1)
- Assessing A Peripheral PulseDocument5 pagesAssessing A Peripheral Pulsecrrfrnc0% (1)
- Decreased Cardiac OutputDocument9 pagesDecreased Cardiac OutputRae AnnNo ratings yet
- What is the initial treatment for heart failure in a 56-year old male with left ventricular dysfunctionDocument51 pagesWhat is the initial treatment for heart failure in a 56-year old male with left ventricular dysfunctionCoral Srinivasa Ramalu100% (1)
- Atrial Systole: The End of DiastoleDocument9 pagesAtrial Systole: The End of DiastoleSophia MahboobNo ratings yet
- Cardio Pulmonary Final FrontierDocument10 pagesCardio Pulmonary Final Frontierdina sharafNo ratings yet
- 9 MedicineDocument351 pages9 MedicineSaravan PramodNo ratings yet
- How to Recognize Congenital Heart Disease in PediatricDocument173 pagesHow to Recognize Congenital Heart Disease in PediatricRidyahningtyas SintowatiNo ratings yet
- Assessment of CVSDocument46 pagesAssessment of CVSdileepkumar.duhs4817No ratings yet
- HyGuru NBME Top ConceptsDocument475 pagesHyGuru NBME Top ConceptsbrownsmilansNo ratings yet
- December 2012 Pnle Pearls of Success Part 6: Medical and Surgical Health Nursing (A)Document11 pagesDecember 2012 Pnle Pearls of Success Part 6: Medical and Surgical Health Nursing (A)Haifi HunNo ratings yet
- Ebook Egans Fundamentals of Respiratory Care 11Th Edition Kacmarek Test Bank Full Chapter PDFDocument40 pagesEbook Egans Fundamentals of Respiratory Care 11Th Edition Kacmarek Test Bank Full Chapter PDFalexandercampbelldkcnzafgtw100% (10)
- Physical DiagnosisDocument42 pagesPhysical DiagnosisKhim Yalong100% (1)
- Assessment of The Heart-Neck Vessels-Peripheral Vessels-PULSEDocument27 pagesAssessment of The Heart-Neck Vessels-Peripheral Vessels-PULSEJonah R. MeranoNo ratings yet
- Emergency Care SeminarDocument136 pagesEmergency Care SeminarSedaka DonaldsonNo ratings yet
- Unit 4 Circulatory SystemDocument157 pagesUnit 4 Circulatory SystemChandan ShahNo ratings yet
- Nur 111 Session 9 Sas 1Document6 pagesNur 111 Session 9 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Cardiology AiimsDocument296 pagesCardiology AiimsDr.vidyaNo ratings yet
- Omd 551 - Part A & Part BDocument17 pagesOmd 551 - Part A & Part Baarthir88100% (2)
- P1 Medworld Academy: Respiratory SystemDocument123 pagesP1 Medworld Academy: Respiratory SystemThenunda തേനുണ്ടNo ratings yet
- Demo On Vital SignsDocument5 pagesDemo On Vital SignsLawrence Cada Nofies100% (3)
- 65-Year-Old Man Chest Pain Diagnosis Acute Aortic DissectionDocument146 pages65-Year-Old Man Chest Pain Diagnosis Acute Aortic DissectionbbdddNo ratings yet
- Pass Your Mrcp Paces in One Attempt-مهممممDocument101 pagesPass Your Mrcp Paces in One Attempt-مهممممpratim dey100% (1)