Professional Documents
Culture Documents
ACLS Algorithms Slide
Uploaded by
hrso0 ratings0% found this document useful (0 votes)
219 views26 pagesacls nih...
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentacls nih...
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
219 views26 pagesACLS Algorithms Slide
Uploaded by
hrsoacls nih...
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 26
Assess responsiveness (speak loudly, gently
shake patient if no trauma - "Annie, Annie,
are you OK?").
Call for help/crash cart if unresponsive.
ABCDs
Airway Open airway, look, listen, and feel for
breathing.
Breathing If not breathing, slowly give 2 rescue
breaths.
Circulation
Check pulse. If pulseless, begin chest compressions at
100/min, 15:2 ratio. Consider no defibrillator nearby
Defibrillation
Attach monitor, determine rhythm. If VF or pulseless
VT: shock up to 3 times. If not, basic CPR.
Then, move quickly to Secondary Survey.
After initial (primary) assessment done
Another set of ABCDs
Airway
Establish and secure an airway device (ETT, LMA,
COPA, Combitube, etc.).
Breathing
Ventilate with 100% O2. Confirm airway placement
(exam, ETCO2, and SpO2). Remember, no
metabolism/circulation = no blue blood to lungs = no
ETCO2.
Circulation
Evaluate rhythm, pulse. If pulseless continue CPR,
obtain IV access, give rhythm-appropriate medications
Differential Diagnosis
Identify and treat reversible causes.
Treatment
Consider bicarb, pacing early
Bicarb (NaHCO3)
Epinephrine 1 mg IV q3-5 min
Atropine 1 mg IV q3-5 min. Max 0.04 mg/kg
Consider possible causes
Hypoxia, Hyperkalemia, Hypothermia, Drug
overdose (e.g., tricyclics), Myocardial Infarction
Consider termination. If patient had >10min
with adequate resucitative effort and no
treatable causes present
Always Primary Survey - Secondary Survey: Confirm
rhythm (check monitor, power, different lead)
Primary Survey
Secondary Survey
assess need for airway, oxygen, IV, monitor, fluids,
vitals, pulse ox
12-lead ECG, Consider Dx
If AV block:
2nd degree (type 2) or 3rd degree: standby TCP, prepare for
transvenous pacing.
If serious signs or symptoms,
Atropine
0.5-1.0 mg IV push q 3-5 min. max 0.04 mg/kg
Pacing
Use transcutaneous pacing (TCP) immediately if sx severe
Dopamine 5-20 g/kg/min
Epinephrine 2-10 g/min
Primary Survey, Secondary Survey: Is patient
stable or unstable?
stable: determine rhythm, treat accordingly
unstable
=chest pain, dyspnea, decreased level of
conciousness, low BP, CHF, AMI
If HR is cause of symptom (almost always HR>150):
cardiovert
Specific Rhythms
Atrial fib/flutter
Narrow-Complex (Supraventricular) Tachycardia
Wide-Complex Tachycardia, Unknown Type
Stable Ventricular Tachycardia
Generally not needed for HR<150.
If HR>150, prepare for immediate cardioversion.
May give brief drug trial.
Steps:
Prepare emergency equipment
Medicate if possible
Cardioversion
monomorphic VT with pulse, PSVT, A fib, A flutter:
100-200-300-360 J* (Synchronized)
may try 50J first for PSVT or A flutter
may use equivalent biphasic (biphasic 70, 120, 150, and 170
J)
if machine unable to synchronize and patient critical,
defibrillate
polymorphic VT: use VT/VF algorithm
Management: Control rate, consider rhythm
cardioversion, and anticoagulate as shown below,
according to Category: 1, 2 or 3
Category 1. Normal EF
Rate control: Ca-blocker or beta-blocker.
Cardiovert:
If onset < 48 hours, consider DC cardioversion OR with
one of the following agents: amiodarone, ibutilide,
procainamide, (flecainide, propafenone), sotalol.
If onset > 48 hours: avoid drugs that may cardiovert
(e.g. amiodarone). Either:
Delayed Cardioversion: anticoagulate adequately x 3 weeks,
then cardioversion, then anticoagulate x 4 weeks
Early Cardioversion: iv heparin, then TEE, then cardioversion
within 24 hours, then anticoagulate x 4 weeks
Transesofageal ekokardiogram
Category 2. EF< 40% or CHF
Rate control:
digoxin, diltizaem, amiodarone
avoid verapamil, beta-blockers, ibutilide,
procainamide (and propafenone/flecainide)
Category 3. WPW A fib
Suggested by: delta wave on resting EKG, very
young patient, HR>300
Avoid adenosine, beta-blocker, Ca-blocker, or
Digoxin
If < 48 hour:
If EF normal: one of the following for both rate control
and cardioversion: amiodarone, procainamide,
propafenone, sotalol, flecainide
If EF abnormal or CHF: amiodarone or cardioversion
If > 48 hour
Medication listed above may be associated with risk of
emboli
Anticoagulate and DC cardioversion as in Category 1.
Sindrom Wolff Parkinson White
If unstable, cardiovert
No cardioversion for stable SVT with low EF.
Management
12-lead ECG, clinical exam
Vagal stimulation, adenosine. Consider esophageal
lead
Treat according to specific rhythm:
PSVT
MAT
Junctional
EF normal
Refleks Vagal
Ca-blocker> beta-blocker> digoxin> DC
Cardioversion.
Consider procainamide, sotalol, amiodarone.
If unstable proceed to cardioversion
EF < 40%, CHF
No Cardioversion. Digoxin or amiodarone or
diltiazem.
If unstable proceed to cardioversion
EF normal: amiodarone, beta-blocker, Ca-
blocker
EF < 40%, CHF: amiodarone
Notes
rare, most commonly misdiagnosed PSVT.
likely digoxin or theophylline OD, catecholamine
state
no cardioversion
If unstable, cardiovert
Attempt to establish specific diagnosis
12 leads, esophageal lead, Clinical info
Note: the use of adenosine to differentiate SVT vs
VT is now de-emphasized.
If unable to make Dx, treat according to EF:
EF normal: DC cardioversion or procainamide or
amiodarone
EF < 40%, CHF: DC cardioversion or amiodarone
Note: no lidocaine and bretylium in protocol
May proceed directly to cardioversion
If not, treat according to morphology:
Monomorphic VT
EF normal: one of the following:
procainamide (2a), sotalol (2a) OR
amiodarone (2b), lidocaine (2b)
EF poor
amiodarone 150 mg iv over 10 min OR lidocaine 0.5-0.75
mg/kg iv push
Synchromized cardioversion
Polymorphic VT
Baseline QT Normal
Possible ischemia (treat) or electrolyte (esp. low K, Mg)
abnormality (correct)
EF normal: betablocker, amiodarone, procainamide, or
sotalol
EF poor
amiodarone 150 mg iv over 10 min
synchromized cardioversion
Prolonged QT baseline (torsade)
Correct electrolyte abnormalities.
Treatment options: magnesium, overdrive
pacing, isoproterenol
Primary Survey, then Secondary Survey: rule
out pseudo-PEA (handheld doppler: look for
cardiac mechanical activities. If present treat
agressively).
Problem
Search for the probable cause ...
Wide QRS: suggests massive myocardial injury,
hyperkalemia, hypoxia, hypothermia
Wide QRS+Slow: consider drug OD (tricyclics, beta-
blockers, Ca-blockers, digoxin)
Narrow complex: suggests intact heart; consider
hypovolemia, infection, PE, tamponade
... and treat as needed
Consider fluid challenge empirically
Consider bicarbonate
hyperkalemia K (Class 1)
bicarbonate responsive acidosis, tricyclic OD, to alkinalize
urine for aspirin OD (Class2a)
prolonged arrest (Class 2b)
not for hypercarbic acidosis
Epinephrine: 1 mg IV q3-5 min
Atropine
If bradycardia, 1 mg IV q3-5 min
max 0.04 mg/kg
If you prefer a mechanistic approach (and are
used to thinking about MAP, CO, SVR, etc.)
think of things that affect forward flow...
Decreased Preload: Hypovolemia, Tamponade,
Tension Pneumothorax
Increased Afterload: Pulmonary Embolus
Decreased Contractility: Hypoxia, Hypothermia,
Acidosis, Myocardial Ischemia
Altered Rate/Rhythm: Hyperkalemia, Drug Overdose
Hypovolemia
Assess: Collapsed vasculature
Tx: Fluids
Hypoxia
Assess: Airway, cyanosis, ABGs
Tx: Oxygen, ventilation
Hydrogen ion (acidosis)
Assess: Diabetic patient, ABGs
Tx: Bicarb 1 mEq/kg, hyperventilation
Hyperkalemia (preexisting)
Assess: Renal patient, EKG, serum K level
Tx: Bicarb, CaCl, albuterol neb, insulin/glucose, dialysis,
diuresis, kayexalate
Hypothermia
Assess: Core temperature
Tx: Hypothermia Algorithm
Tablets/toxins overdose
Assess: Hx of medications, drug use
Tx: Treat accordingly
Tamponade, cardiac
Assess: No pulse w/ CPR, JVD, narrow pulse pressure
prior to arrest
Tx: Pericardiocentesis
Tension pneumothorax
Assess: No pulse w/ CPR, JVD, tracheal deviation
Tx: Needle thoracostomy
Thrombosis, coronary
Assess: History, EKG
Tx: Acute Coronary Syndrome algorithm
Thrombosis, pulmonary embolism
Assess: No pulse w/ CPR, JVD
Tx: Thrombolytics, surgery
Remember: initial stacked shocks are part of the
primary survey
Implement the secondary survey after your stacked
shocks.
Meds: Shock-drug-shock-drug-shock pattern.
Continue CPR while giving meds, and shock (360J or
150J if biphasic) within 30-60 seconds. Evaluate
rhythm and check for pulse immediately after
shocking.
Epi or vasopressin big drugs (may give either one as
first choice).
If VF/PVT persists, may move on to antiarrhythmics and
sodium bicarb
max out one antiarrhythmic before proceeding to the next
in order to limit pro-arrhythmic drug-drug interactions.
Shock 200J*
If VF or VT is shown on monitor: shock immediately.
Do not lift paddles from chest after shocking -
simultaneously charge at next energy level and evaluate
rhythm.
Shock 200-300J*
If VF or VT persists on monitor, shock immediately.
Do not check pulse, do not continue CPR, do not lift
paddles from chest.
After shocking, simultaneously charge at next energy
level and evaluate rhythm.
Shock 360J*
If VF or VT persists, shock immediately.
Epinephrine
1 mg IV q3-5 min.
High dose epinephrine is no longer recommended
Vasopressin
40 U IV
one time dose (wait 5-10 minutes before starting epi).
Preferred first drug?
Shock 360J*
Amiodarone (Class 2b)
300mg IV push.
May repeat once at 150mg in 3-5 min
max cumulative dose = 2.2g IV/24hrs
Shock 360J*
Magnesium Sulfate (Class 2b)
1-2 g IV (over 2 min) for suspected
hypomagnesemia or torsades de pointes
(polymorphic VT)
Shock 360J*
Bicarbonate
1 mEq/kg IV for reasons below:
Class 1: hyperkalemia
Class 2a: bicarbonate-responsive acidosis, tricyclic
OD, to alkinalize urine for aspirin OD
Class 2b: prolonged arrest
Not for hypercarbia-related acidosis, nor for routine
use in cardiac arrest
You might also like
- ACLS Algorithms (2011)Document6 pagesACLS Algorithms (2011)senbonsakuraNo ratings yet
- ACLS Official GuideDocument11 pagesACLS Official GuideICU RSPGNo ratings yet
- ACLS Simplify AlgorithmDocument6 pagesACLS Simplify AlgorithmKristine Monforte Coma UritaNo ratings yet
- ACLS Algorithms Adult 2010 Revised May 31 2011Document12 pagesACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614No ratings yet
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Heart Block, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHeart Block, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- CCU Clinical GuidelinesDocument63 pagesCCU Clinical GuidelinesHAMMYER ALROKHAMINo ratings yet
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDocument34 pagesArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212No ratings yet
- ICE DrugsDocument2 pagesICE DrugsRichelle FrondaNo ratings yet
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDocument49 pagesAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamNo ratings yet
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- HO - Burns Environmental EmergenciesDocument7 pagesHO - Burns Environmental EmergenciesSteven Paul DaclesNo ratings yet
- ACLS Algorithm Pulse No Yes: Stable Patient Unstable Patient Stable PatientDocument1 pageACLS Algorithm Pulse No Yes: Stable Patient Unstable Patient Stable PatientAhmed AlkhaqaniNo ratings yet
- Shock: Shout For Help/Activate Emergency ResponseDocument6 pagesShock: Shout For Help/Activate Emergency ResponseandiyanimalikNo ratings yet
- CPR ACLS Study GuideDocument18 pagesCPR ACLS Study GuideJohn Phamacy100% (1)
- Drugs and Defibrillation: Department of Anesthesiology & Reanimation General Hospital TasikmalayaDocument20 pagesDrugs and Defibrillation: Department of Anesthesiology & Reanimation General Hospital TasikmalayaAfrida Sahestina100% (1)
- Selected Nursing Diagnoses and Interventions For Patients With DysrhythmiasDocument19 pagesSelected Nursing Diagnoses and Interventions For Patients With Dysrhythmiaslanie_jecielNo ratings yet
- Adenosine: Rapid IV PushDocument4 pagesAdenosine: Rapid IV PushsabboNo ratings yet
- Sample Acls For DummiesDocument3 pagesSample Acls For DummiesTodd Cole100% (1)
- Intubation ChecklistDocument2 pagesIntubation ChecklistDaniel CrookNo ratings yet
- ACLS ChartDocument1 pageACLS ChartJev DespiNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyNo ratings yet
- Rhythm Recognition - ACLS Medical Training 1Document9 pagesRhythm Recognition - ACLS Medical Training 1Catalina BorquezNo ratings yet
- ToxidromesDocument1 pageToxidromesMayer Rosenberg100% (7)
- Nervous System AlterationsDocument45 pagesNervous System AlterationsMajesty ParkerNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- ACLS NotesDocument3 pagesACLS Notessaxmanwrv0% (1)
- ECG Dysrhthmias IIIDocument31 pagesECG Dysrhthmias IIIAmani KayedNo ratings yet
- HW InotropesDocument3 pagesHW InotropesNatalie YeohNo ratings yet
- Emergency Lecture PDFDocument57 pagesEmergency Lecture PDFDuane Liloc100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Topic Discussion Heart Failure MedicationsDocument7 pagesTopic Discussion Heart Failure Medicationsapi-385309917No ratings yet
- 1008 1400 ACLS - StudyGuide Print PDFDocument54 pages1008 1400 ACLS - StudyGuide Print PDFWaqar HassanNo ratings yet
- BLS SummaryDocument2 pagesBLS Summaryreyes markNo ratings yet
- Hemodynamic Drug InfusionsDocument45 pagesHemodynamic Drug InfusionsDawit MucheNo ratings yet
- Introduction To ECG RhythmsDocument59 pagesIntroduction To ECG RhythmsIvona RagužNo ratings yet
- Chest Tube Explanation by AllnursesDocument3 pagesChest Tube Explanation by AllnursesYemaya84No ratings yet
- Normal Ranges Vital Signs 2017Document2 pagesNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- Acls LectureDocument15 pagesAcls LectureVincent BautistaNo ratings yet
- Nursing Responsibilities in Handling AntibioticsDocument4 pagesNursing Responsibilities in Handling Antibioticsrichardmd20% (1)
- Pic PALS PDFDocument57 pagesPic PALS PDFJimcyNo ratings yet
- ACLS Training - Most Important Points To RememberDocument5 pagesACLS Training - Most Important Points To RememberEman ElzeftawyNo ratings yet
- Grady EMS Drug List 2017 FINALDocument20 pagesGrady EMS Drug List 2017 FINALThomas LeachNo ratings yet
- Practice StripsDocument9 pagesPractice StripsErica Yamamoto50% (4)
- Drugs in Cardiac EnmergenciesDocument94 pagesDrugs in Cardiac EnmergenciesVijayan VelayudhanNo ratings yet
- Basic EKG Interpretation Exam AnswersDocument3 pagesBasic EKG Interpretation Exam AnswerstwdroppointNo ratings yet
- MegaCode Kelly TSMDocument35 pagesMegaCode Kelly TSMWagner Tumialan100% (1)
- Hyper-coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHyper-coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Acls DrugsDocument10 pagesAcls DrugsChintami Octavia100% (1)
- KonsulDocument1 pageKonsulhrsoNo ratings yet
- ACLS Drugs: o o o o o oDocument3 pagesACLS Drugs: o o o o o ohrsoNo ratings yet
- ACLS AlgorithmsDocument13 pagesACLS AlgorithmsHap SchneiderNo ratings yet
- Supracondylar FractureDocument24 pagesSupracondylar FracturehrsoNo ratings yet
- Mandala of HeathDocument1 pageMandala of HeathhrsoNo ratings yet
- Drug Interaction Chart PrescriptionDocument7 pagesDrug Interaction Chart PrescriptionSimona LipanNo ratings yet
- Ling Wu Case NotesDocument3 pagesLing Wu Case NotesOana Maria Grigore77% (13)
- Student Tox LectureDocument49 pagesStudent Tox Lecturelenin_villaltaNo ratings yet
- Heparin and WarfarinDocument2 pagesHeparin and WarfarinBaeyer100% (1)
- Direct-to-Consumer Pharmaceutical AdvertisingDocument10 pagesDirect-to-Consumer Pharmaceutical AdvertisingNag ArjunNo ratings yet
- Medication Management in Older Adults - A Concise Guide For Clinicians - S. Koch, Et Al., (Springer, 2010) WWDocument143 pagesMedication Management in Older Adults - A Concise Guide For Clinicians - S. Koch, Et Al., (Springer, 2010) WWGeorgianaRamonaNo ratings yet
- Medication Calculations Part 2Document7 pagesMedication Calculations Part 2Karla FralalaNo ratings yet
- Maged 2015Document185 pagesMaged 2015engy6nagyNo ratings yet
- Ferrous Sulfate 60 MLDocument1 pageFerrous Sulfate 60 MLRomel LeoNo ratings yet
- Herniated Nucleus Pulposus (Report) - 2Document27 pagesHerniated Nucleus Pulposus (Report) - 2Angelu Gabrielle CastroNo ratings yet
- Medication Conversion ChartDocument2 pagesMedication Conversion ChartIlinca mirnoviciNo ratings yet
- What We Need From You: Please Return Page 2 Via Fax To (512) 738-8397Document2 pagesWhat We Need From You: Please Return Page 2 Via Fax To (512) 738-8397Tàrár ŁàráibNo ratings yet
- Therapeutics in Endodontics: DR Mohamed RabieDocument75 pagesTherapeutics in Endodontics: DR Mohamed RabieAbdelrahman GalalNo ratings yet
- Psychiatric MedicationDocument22 pagesPsychiatric MedicationSofia Centro TaerNo ratings yet
- Discharge Planning PaperDocument4 pagesDischarge Planning Paperapi-252001755100% (1)
- Erythema MultiformeDocument159 pagesErythema MultiformeWendy EvansNo ratings yet
- Laporan Gufar Bulan April 2019Document235 pagesLaporan Gufar Bulan April 2019juerNo ratings yet
- First Case Study CA2Document5 pagesFirst Case Study CA2KZNo ratings yet
- Chapter 21 Antidepressant AgentsDocument4 pagesChapter 21 Antidepressant AgentsNicolle Lisay IlaganNo ratings yet
- AtivanDocument1 pageAtivanSheri490No ratings yet
- Neuropsychiatry High Yield Notes PDFDocument6 pagesNeuropsychiatry High Yield Notes PDFTolaniNo ratings yet
- Final ReportDocument53 pagesFinal ReportParth Gandhi100% (1)
- Chronic Pain SAQ'sDocument52 pagesChronic Pain SAQ'sNaser AhmedNo ratings yet
- LiverpoolSedation ManagementDocument9 pagesLiverpoolSedation ManagementTheresia Avila KurniaNo ratings yet
- Dosage & Solution (Pharma)Document8 pagesDosage & Solution (Pharma)Wenn Joyrenz ManeclangNo ratings yet
- Sop For Controlled DrugsDocument75 pagesSop For Controlled DrugsBalaji Pharmacy - GMNo ratings yet
- Spring II 2015 Term - Practice Exam 1 - Med Math CalDocument7 pagesSpring II 2015 Term - Practice Exam 1 - Med Math CalArashnNo ratings yet
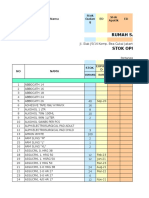
- Stock Opname Bulan September 2018Document138 pagesStock Opname Bulan September 2018Miftah RamadhanNo ratings yet
- Canamed 2011Document5,256 pagesCanamed 2011Alina IamandiNo ratings yet
- Barrier For Ocular Drug Delivery SystemDocument15 pagesBarrier For Ocular Drug Delivery SystemVeenu ChaudharyNo ratings yet